Possibility of migraine-free days*2–4
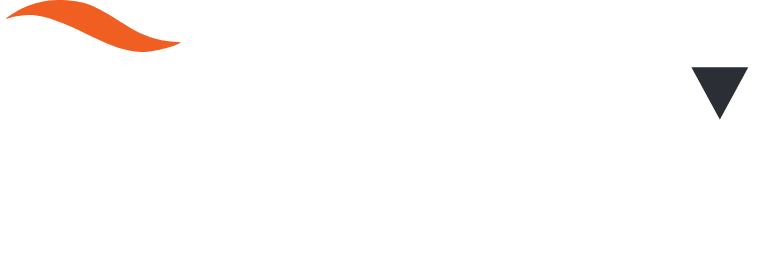
EPISODIC MIGRAINE, 60 MG | 52-WEEK OPEN-LABEL SAFETY STUDY
Efficacy endpoint:
At Weeks 49–52, there were
0 migraine attacks in2
48.4%
of remaining patients receiving
AQUIPTA™ 60 mg once daily2
Efficacy endpoints for long-term efficacy evaluation were not classified as primary, secondary or additional endpoints. Data from an open-label safety study that randomised 744 patients 5:2 to receive either AQUIPTA™ 60 mg (N=546) or standard of care migraine prevention medication (n=198). Adults from the previous Phase 2b/3 trial, who re-established study eligibility, and de novo patients were included. Participants had 4–14 migraine days in the 28-day baseline period. Efficacy measures, changes from baseline in least squares mean monthly migraine days, moderate/severe headache days, mean monthly acute medication use days and the proportion of responders based on reductions in monthly migraine days were evaluated using the mITT population and a mixed-effects model for repeated measures. Clinical efficacy outcomes were only collected from the AQUIPTA™ arm by eDiary data. Of N=546 randomised to the AQUIPTA™ 60 mg arm, n=521 were included in the mITT population and n=373 completed 52 weeks’ treatment.2 In an open-label extension with observed data, there is potential for enrichment of the long-term data as those who remain in the study generally fare better than those who discontinue.
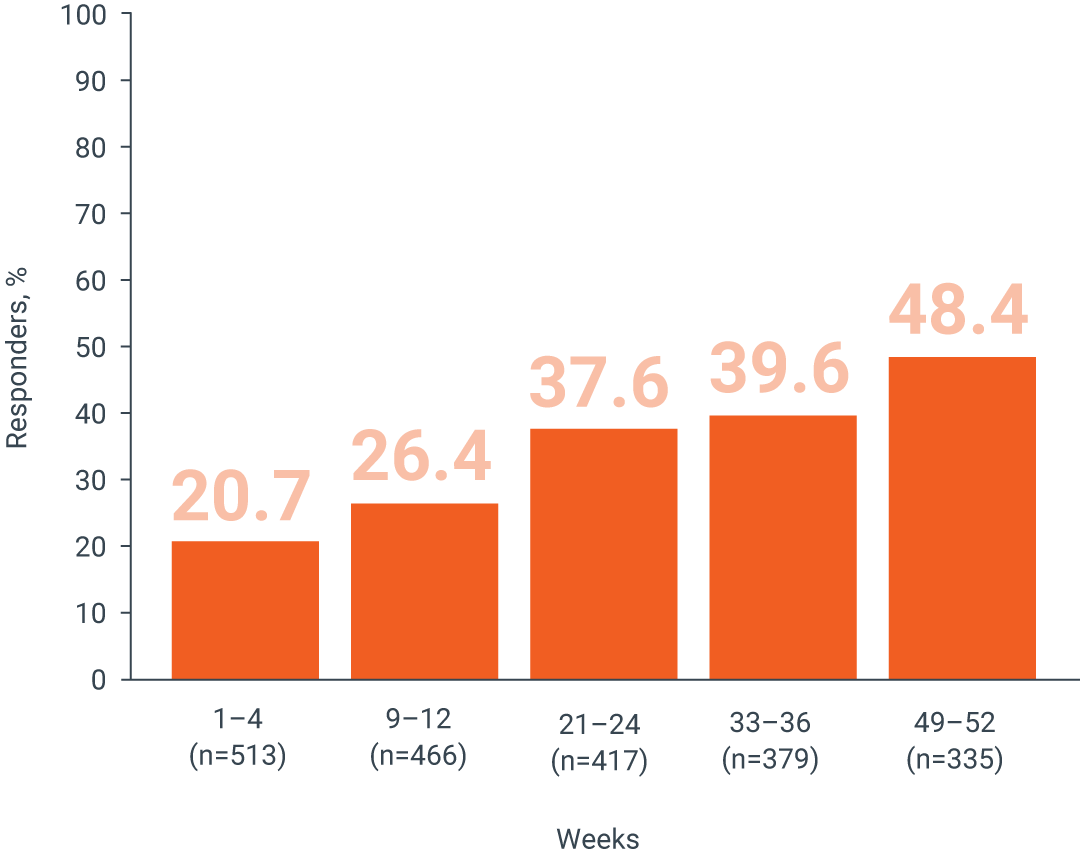
EPISODIC MIGRAINE, 60 MG | ADVANCE PIVOTAL PREVENTION STUDY†
Predefined exploratory endpoint:
In the last month of the study period (Weeks 9–12),
there were 0 migraine attacks in3
27.7%
of patients treated with AQUIPTA™
60 mg once daily3
vs.
11.2%
of patients treated
with placebo3
p<0.0013
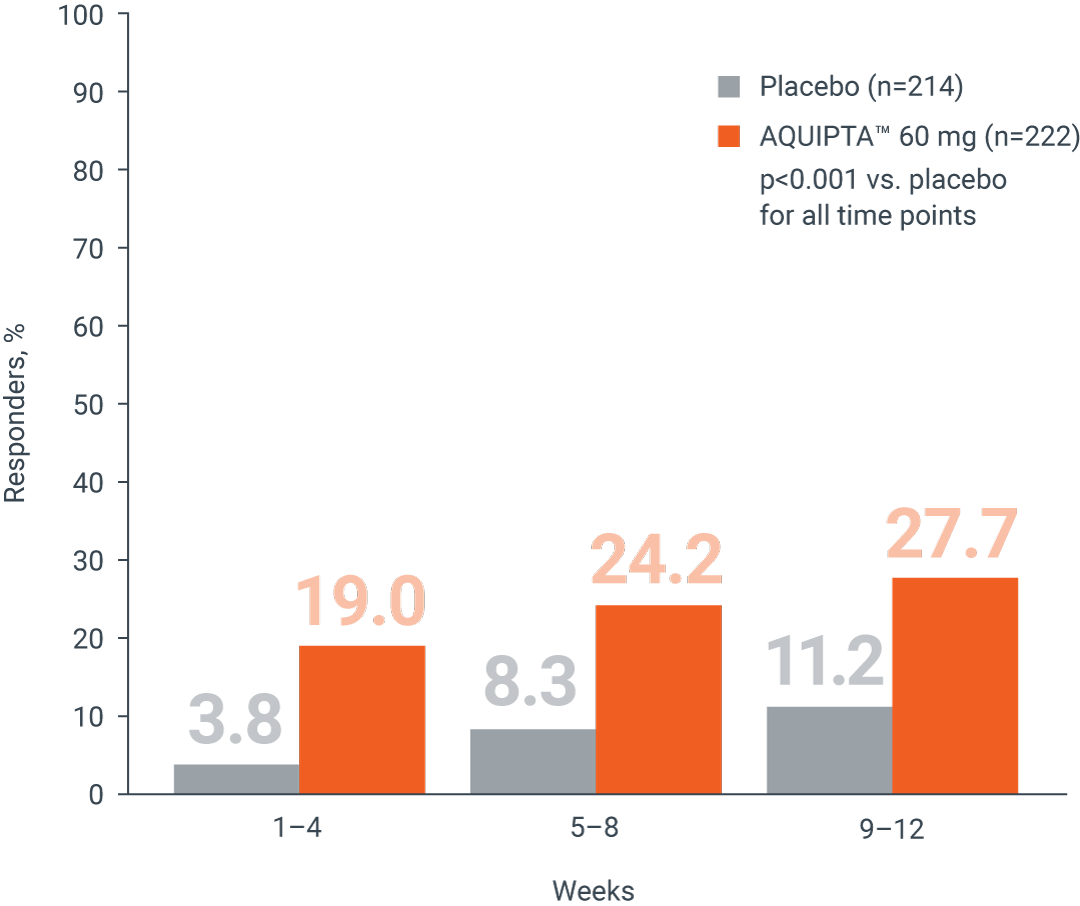
CHRONIC MIGRAINE, 60 MG | PROGRESS PIVOTAL PREVENTION STUDY‡
Additional endpoint:
In the last month of the study period (Weeks 9–12),
there were 0 migraine attacks in4
7.4%
of patients treated with AQUIPTA™
60 mg once daily4
vs.
2.6%
of patients treated
with placebo4
p<0.05§4
IE, Ireland; mITT, modified intent-to-treat.
*Free from migraine defined as 0 attacks in a defined period. †A secondary analysis of a Phase 3, double-blind, placebo-controlled randomised clinical trial (ADVANCE) evaluating the efficacy and safety of AQUIPTA™ for the preventive treatment of episodic migraine.3 The mITT population included all participants who received ≥1 dose of AQUIPTA™ or placebo and had evaluable baseline, and ≥1 4-week post-baseline period, eDiary data.3 ‡An additional analysis of a Phase 3, double-blind, placebo-controlled, randomised clinical trial (PROGRESS) evaluating the efficacy and safety of AQUIPTA™ for the preventive treatment of chronic migraine.4 §Nominal p-value, without adjustment for multiplicity.4
References:
- AQUIPTA™ (atogepant) IE Summary of Product Characteristics. August 2023.
- Ashina M, et al. Headache. 2023;63(1):79–88.
- Lipton RB, et al. JAMA Netw Open. 2022;5(6):e2215499.
- Lipton RB, et al. Migraine Trust International Symposium (MTIS) 2022, 8–11 September; London, UK.
ALL-AQP-230003 March 2024