Preventive treatment for migraine that is generally well tolerated vs. placebo2–4
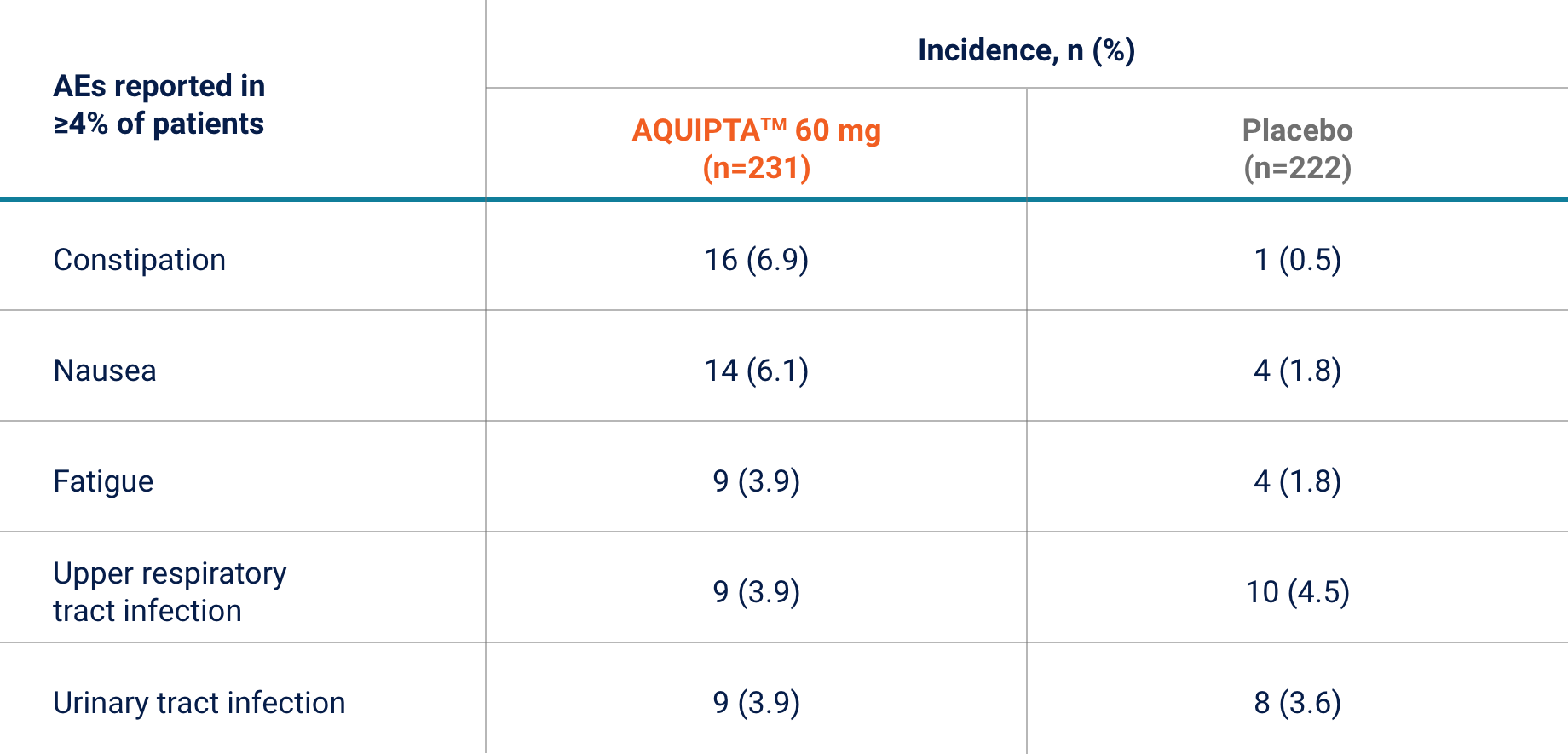
EPISODIC MIGRAINE, 60 MG | ADVANCE PIVOTAL PREVENTION STUDY*
In the 12-week episodic migraine study, AQUIPTA™ 60 mg was generally well tolerated vs. placebo across 12 weeks.*2
Safety population: all randomly assigned participants who received at least one dose of AQUIPTA™ or placebo.2
Rates of AEs leading to discontinuation were similar in both study arms:2
Rates of AEs related to AQUIPTA™ 60 mg were 19.5%
(n=45/231) and 9% (n=20/222) for placebo†2
No serious AEs related to treatment were reported in
patients in the AQUIPTA™ 60 mg or placebo arm†2
AQUIPTA™ can offer your patients with episodic migraine:
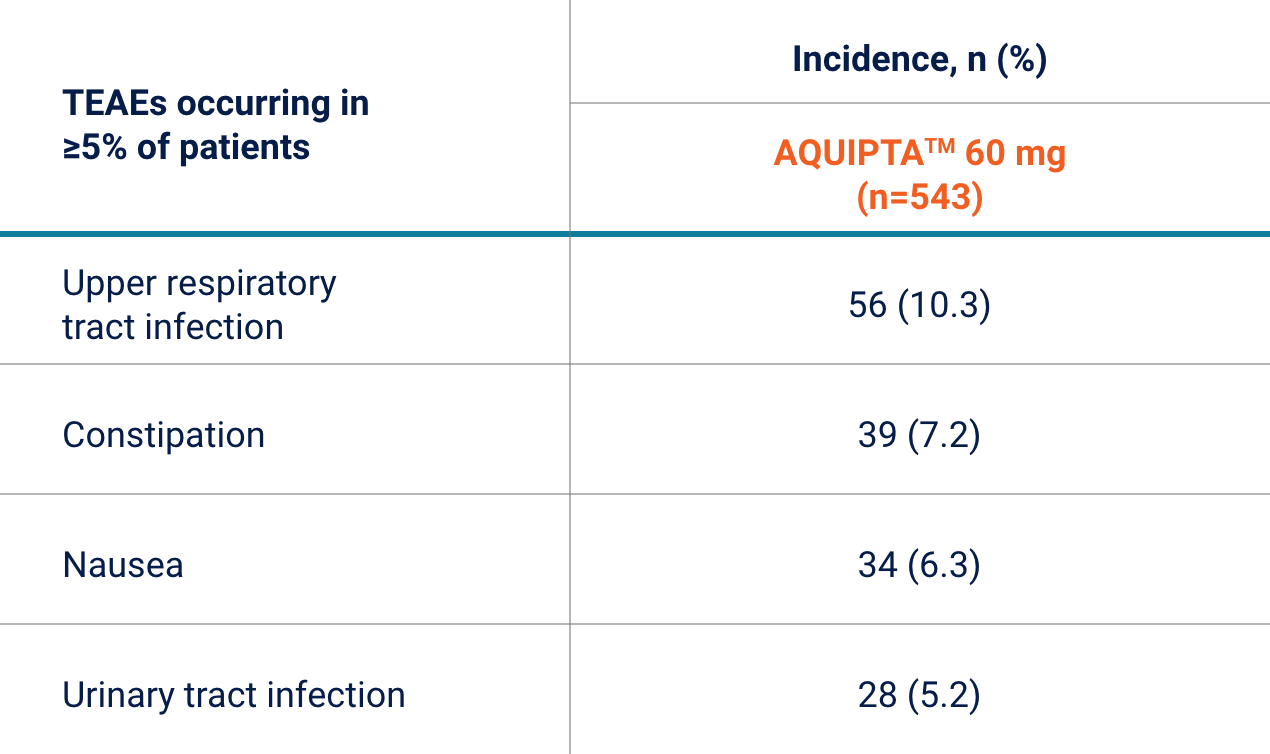
A 52-week, multicentre, randomised, open-label trial to examine the long-term safety, tolerability and efficacy of AQUIPTA™ 60 mg for the prevention of episodic migraine.4
- TEAEs occurred in 364/543 (67%) of patients treated with AQUIPTA™ 60 mg4
- The majority were mild (n=140/543, 28.5%) or moderate (n=187/543, 34.4%) in severity. Severe TEAEs occurred in 6.8% (n=37/543) patients4
- Most cases of constipation were mild to moderate in severity with one patient reporting a severe case. This did not result in discontinuation, was downgraded to ‘mild’ on Day 96 and resolved on Day 1264
- Serious TEAEs were reported in 4.4% (n=24/543) of AQUIPTA™ treated patients4
With AQUIPTA™, you can offer efficacious and
generally well tolerated migraine prevention2–4
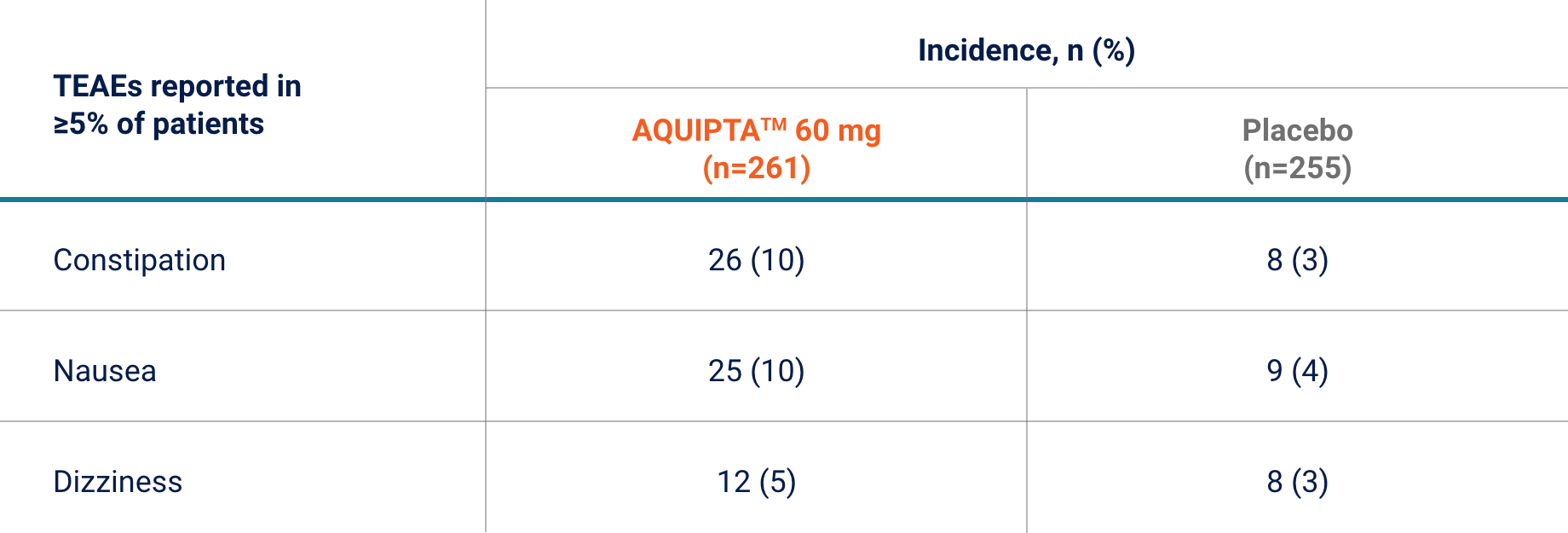
EPISODIC MIGRAINE, 60 MG | PROGRESS PIVOTAL PREVENTION‡
In the 12-week chronic migraine study, AQUIPTA™ 60 mg was generally well tolerated vs. placebo across 12 weeks.‡3
Safety population: all randomly assigned participants who received at least one dose of AQUIPTA™ or placebo.3
Rates of AEs leading to discontinuation were similar in both study arms:3
Serious TEAEs were reported in 3% (n=7/261) of patients in the AQUIPTA™ 60 mg arm
(vs. n=3/255, 1% in placebo arm)3
None of these were considered related to the study drug3
With AQUIPTA™, you can offer efficacious and
generally well tolerated migraine prevention2–4
AE, adverse event; ICHD, International Classification of Headache Disorders; IE, Ireland; mITT, modified intent-to-treat; TEAE, treatment-emergent adverse event.
*Pivotal study that evaluated AQUIPTA™ for the prophylaxis of episodic migraine that enrolled patients who met ICHD criteria for a diagnosis of migraine with or without aura. Patients with myocardial infarction, stroke, or transient ischaemic attacks within 6 months prior to screening were excluded.1,2 †The relatedness of AEs to AQUIPTA™ or placebo was determined by the investigator.2 ‡Pivotal study that evaluated AQUIPTA™ for the prophylaxis of chronic migraine that enrolled patients who met ICHD criteria for chronic migraine. Patients with myocardial infarction, stroke, or transient ischaemic attacks within 6 months prior to screening were excluded.1,3 §Data from an open-label safety study that randomised 744 patients 5:2 to receive either AQUIPTA™ 60 mg (N=546) or standard of care migraine prevention medication (n=198). Adults from the previous Phase 2b/3 trial, who re-established study eligibility, and de novo patients were included. Participants had 4–14 migraine days in the 28-day baseline period. Efficacy measures, changes from baseline in least squares mean monthly migraine days, moderate/severe headache days, mean monthly acute medication use days and the proportion of responders based on reductions in monthly migraine days were evaluated using the mITT population (n=521 AQUIPTA™-treated patients) and a mixed-effects model for repeated measures. Efficacy endpoints for long-term efficacy evaluation were not classified as primary, secondary or additional endpoints. Clinical efficacy outcomes were only collected from the AQUIPTA™ arm by electronic diary (eDiary) data.4 In an open-label extension with observed data, there is potential for enrichment of the long-term data as those who remain in the study generally fare better than those who discontinue.
References:
- AQUIPTA™ (atogepant) IE Summary of Product Characteristics. August 2023.
- Ailani J, et al. N Engl J Med. 2021;385:695–706.
- Pozo-Rosich P, et al. Lancet. 2023;402(10404):775–785 (Supplementary Appendix).
- Ashina M, et al. Headache. 2023;63(1):79–88.
ALL-AQP-230003 March 2024