SKYRIZI (risankizumab) is an IL-23/p19 inhibitor indicated for the treatment of moderate to severe plaque psoriasis in adults who are candidates for systemic therapy. SKYRIZI, alone or in combination with MTX, is also indicated for the treatment of active psoriatic arthritis in adults who have had an inadequate response or who have been intolerant to one or more DMARDs.1
SKYRIZI: An IL-23/p19 inhibitor2-7
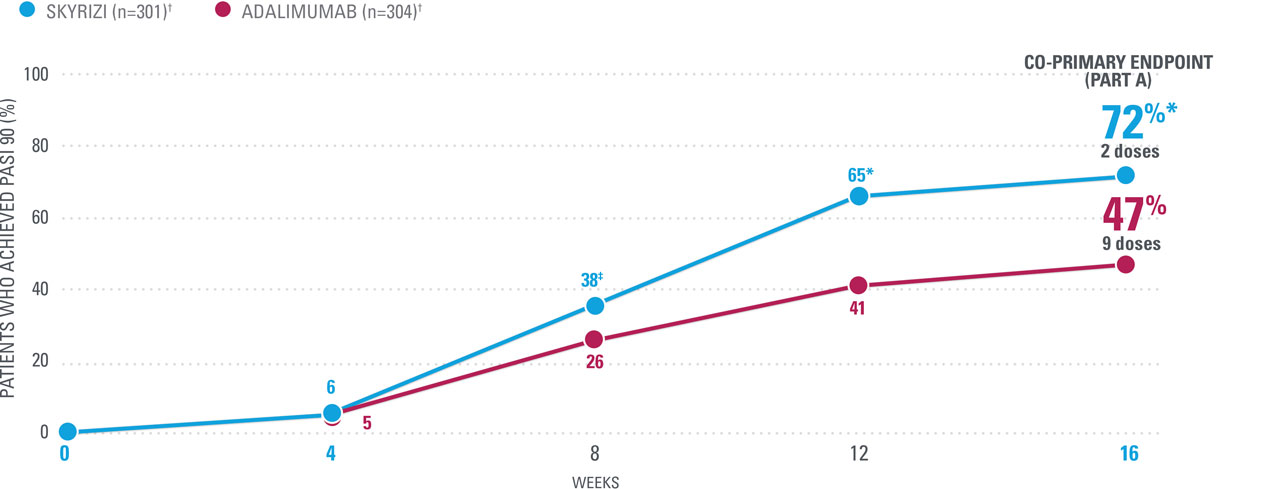
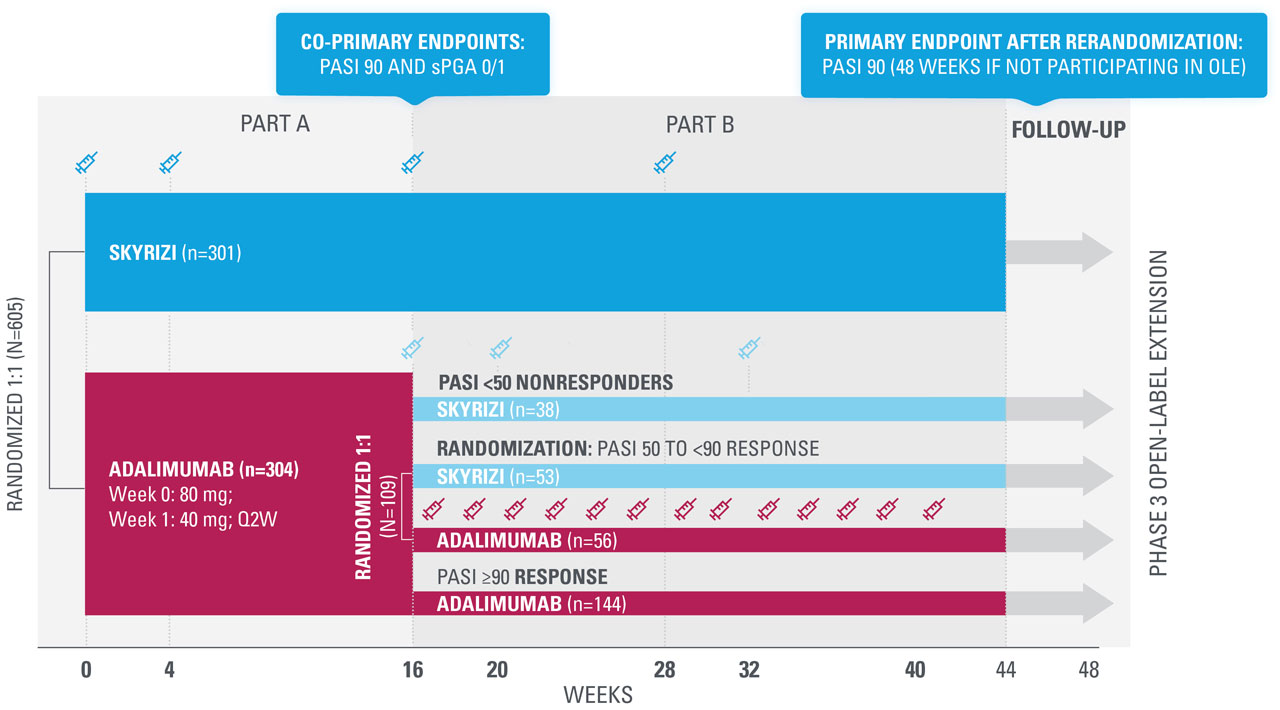
IMMvent: SKYRIZI vs adalimumab in patients with moderate to severe PsO
HIGH LEVELS OF CLEARANCE in more patients compared to adalimumab
SUPERIOR AT WEEK 16: 72% OF SKYRIZI PATIENTS ACHIEVED PASI 90 VS 47% ADALIMUMAB (NRI)1,16*
| Co-primary endpoint: 84% of patients achieved sPGA 0/1 at Week 16 with SKYRIZI vs 60% adalimumab (P<0.0001).16 |
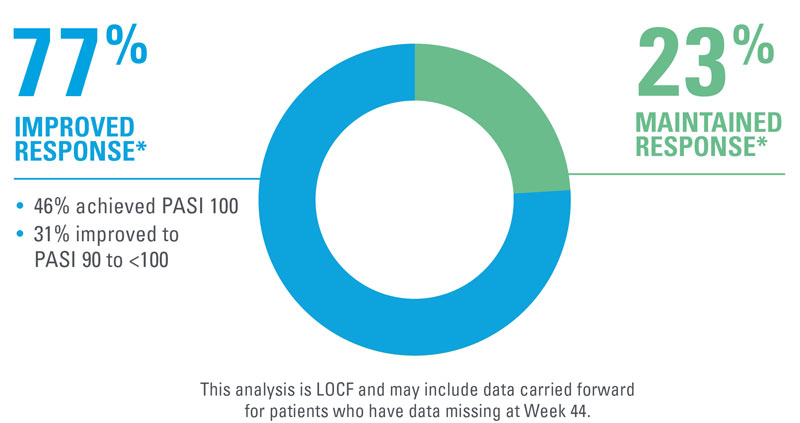
In patients with a response of PASI ≥50 to <90 after 16 weeks of adalimumab treatment (Part B)
3X MORE PATIENTS ACHIEVED PASI 90 AT WEEK 44 AFTER SWITCHING TO SKYRIZI THAN THOSE WHO STAYED ON ADALIMUMAB1,16*
RERANDOMIZATION: Adalimumab patients achieving PASI ≥50 to <90
| * | P<0.0001 vs adalimumab. |
| † | SKYRIZI doses denoted in blue: Patients were stratified by weight (≤100 kg vs >100 kg) and prior TNF inhibitor exposure (no vs yes) and randomized 1:1 to receive 150 mg SKYRIZI (Weeks 0, 4, and 16) or adalimumab (80 mg at Week 0, 40 mg every other week [EOW]) from Week 1. |
| ‡ | P=0.0012 vs adalimumab; §P=0.0142 vs adalimumab; llP=0.0001 vs adalimumab. |
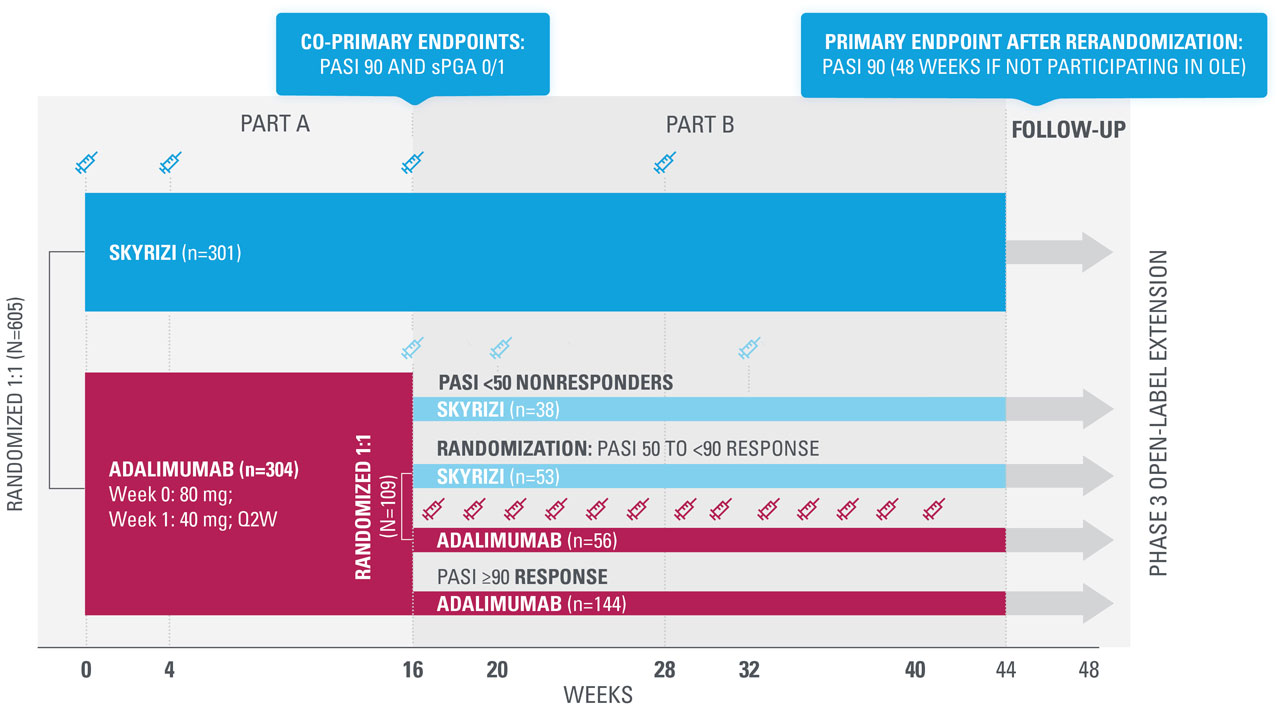
| Adalimumab-treated patients achieving PASI 50 to <90 at Week 16 were stratified by weight and prior TNF inhibitor exposure and rerandomized 1:1 to either continue adalimumab EOW until Week 41 or switch to SKYRIZI (Weeks 16, 20, and 32). | |
| Inadequate or partial response in the IMMvent study was defined as PASI ≥50 to <90 at Week 16 in patients receiving adalimumab. |
IMMvent Phase 3 study design16
A 44-week, randomized comparative study vs adalimumab in patients with moderate to severe chronic plaque psoriasis (N=605)
Nothing more than 4 INJECTIONS PER YEAR after initiation doses for both PsO and PsA patients1*
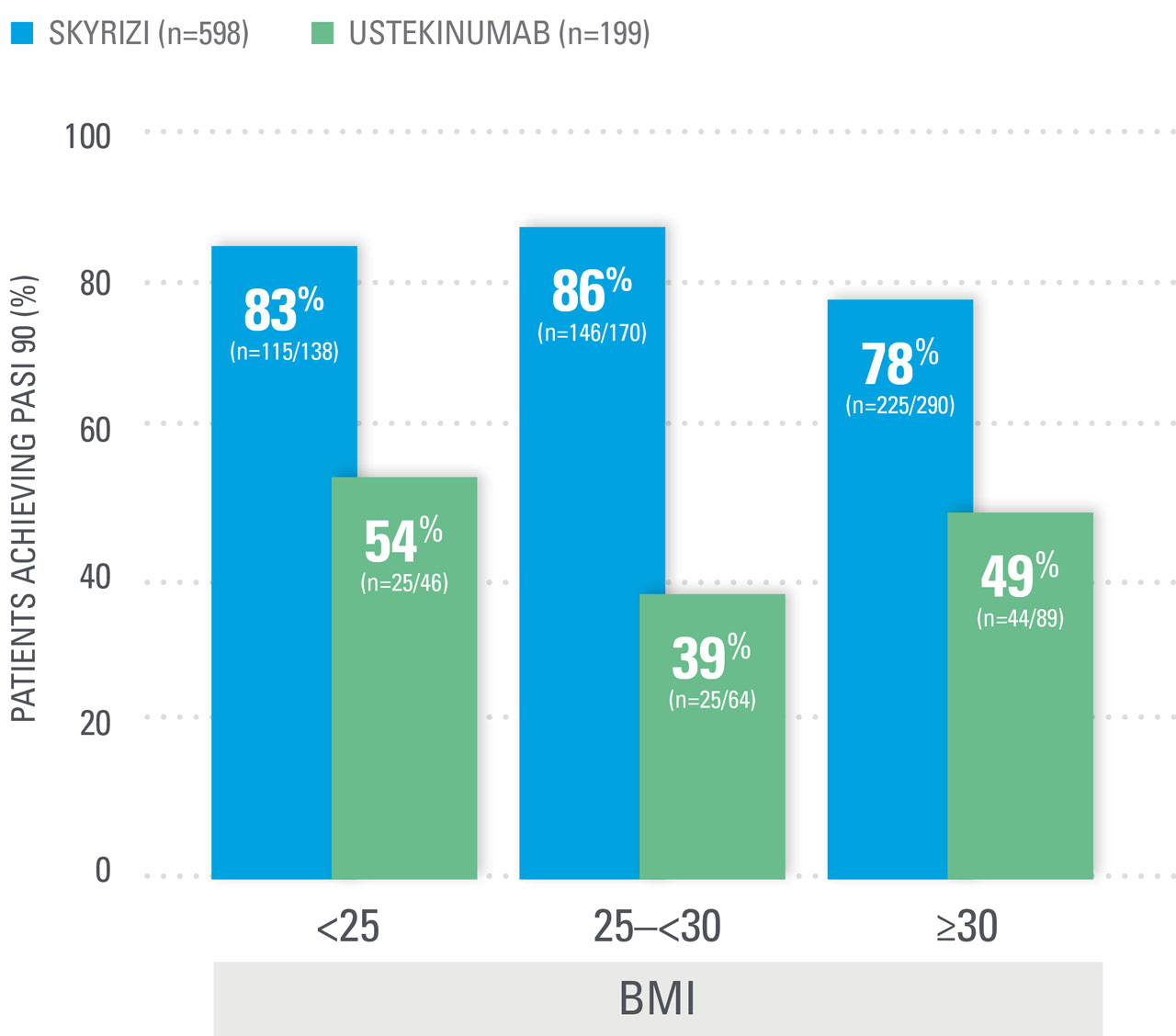
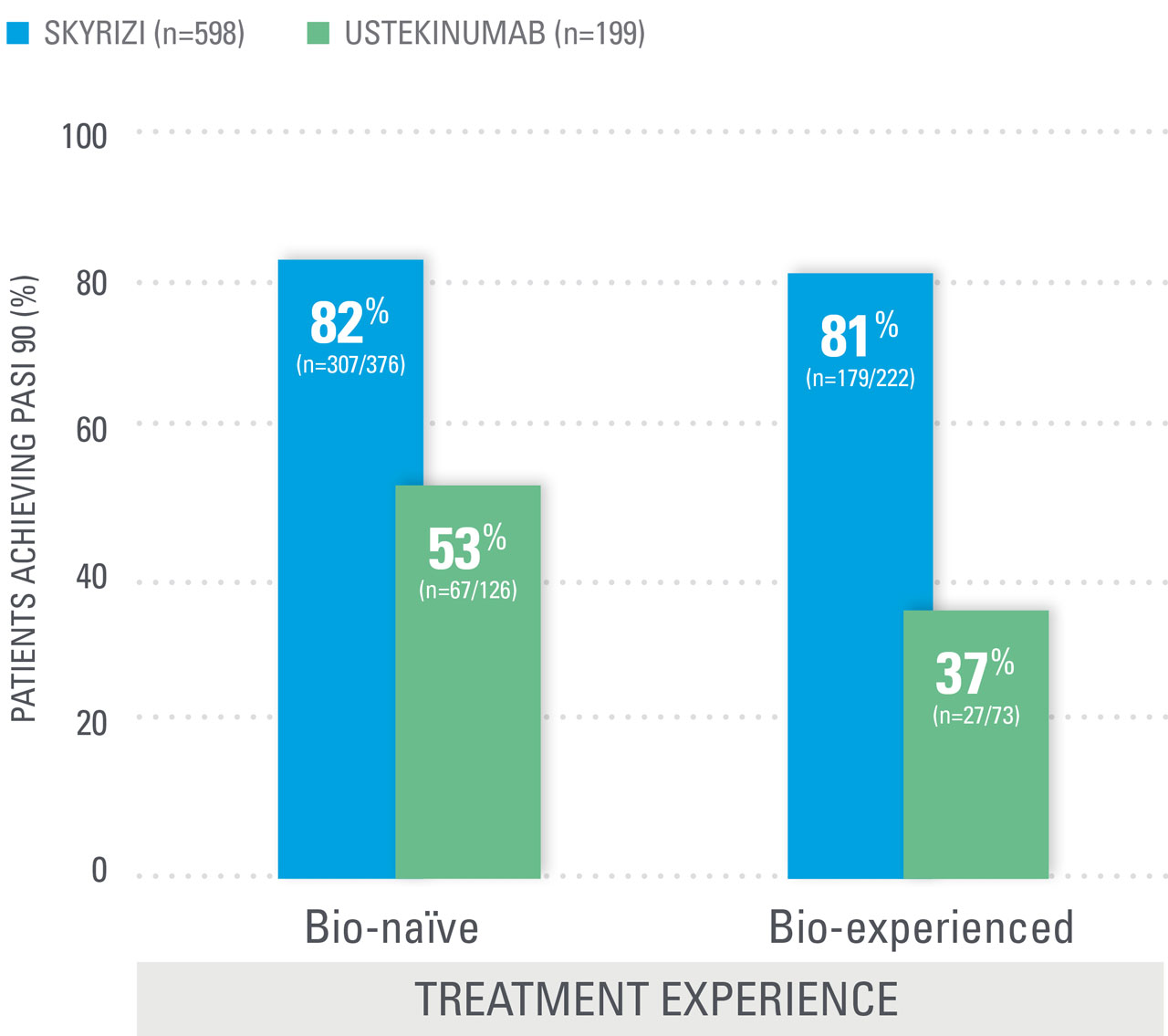
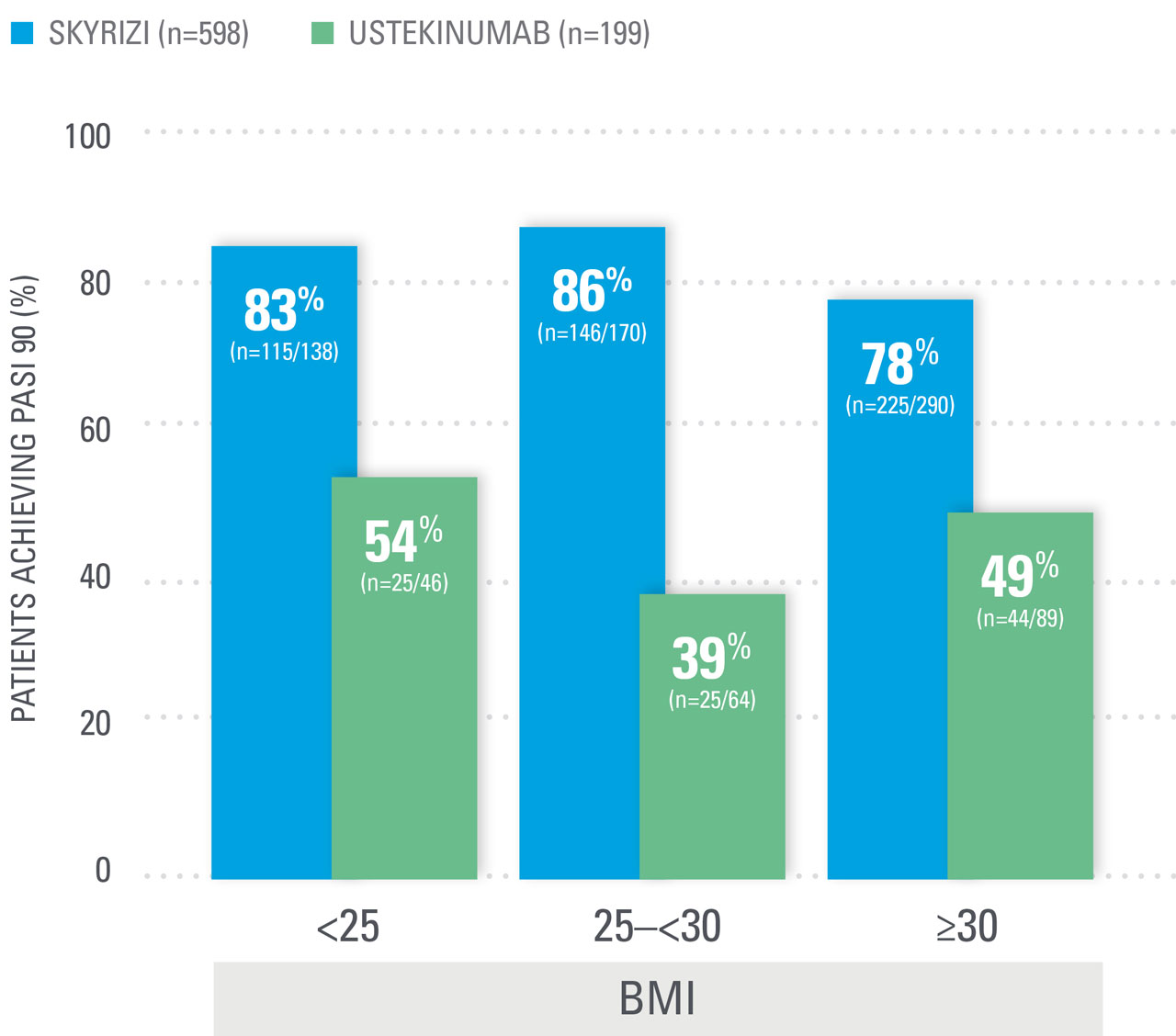
NO DOSE ADJUSTMENT regardless of baseline characteristics, including BMI and weight1,11,12†
- SKYRIZI is dosed 150 mg (one 150-mg subcutaneous injection) at Week 0, Week 4, and every 12 weeks thereafter for adult patients with moderate to severe PsO or active PsA.1
- Low rate of injection site reactions at Week 16 (based on an analysis of 5 PsO clinical trials: SKYRIZI 1.5% vs placebo 1.0%)13
—In a long-term PsO analysis (up to 8.8 years), rates of injection site reactions were low for SKYRIZI patients (2.8 E/100 PY).14‡
Consideration should be given to discontinuing treatment in patients who have shown no response after 16 weeks of treatment. Some patients with initial partial response may subsequently improve with continued treatment beyond 16 weeks.
| * | Maintenance dosing (one 150-mg subcutaneous injection/dose) every 12 weeks following a starter dose at Week 0 and Week 4. If a dose is missed, the dose should be administered as soon as possible. Thereafter, dosing should be resumed at the regular scheduled time. |
| † | Risankizumab clearance and volume of distribution increase as body weight increases, which may result in reduced efficacy in subjects with high body weight (>130 kg). However, this observation is based on a limited number of subjects. |
| ‡ | Week 16 (5-study pool) and long-term (median duration of treatment 4.1 years [ranging from 81 days to 8.8 years] 20-study pool) represent different pools of patients with varying lengths of treatment exposure included in the long-term data set.14 |
SKYRIZI one injection per dose:
SAME EFFICACY AND SAFETY PROFILE
Same active ingredient | Demonstrated bioequivalence1
NOW EVEN SIMPLER WITH
Note to Affiliate: “New” is a regulated term to be used for up to one year per EFPIA code of practice. Please evaluate use of "Now" in relation to 150 mg presentation, given dates of availability in your country and local requirements.
SKYRIZI 150 mg bioequivalence data1
Bioequivalence was demonstrated between a single SKYRIZI 150-mg injection and two SKYRIZI 75-mg injections in a prefilled syringe. Bioeqivalence was also demonstrated between SKYRIZI 150 mg in a prefilled syringe and a prefilled pen.
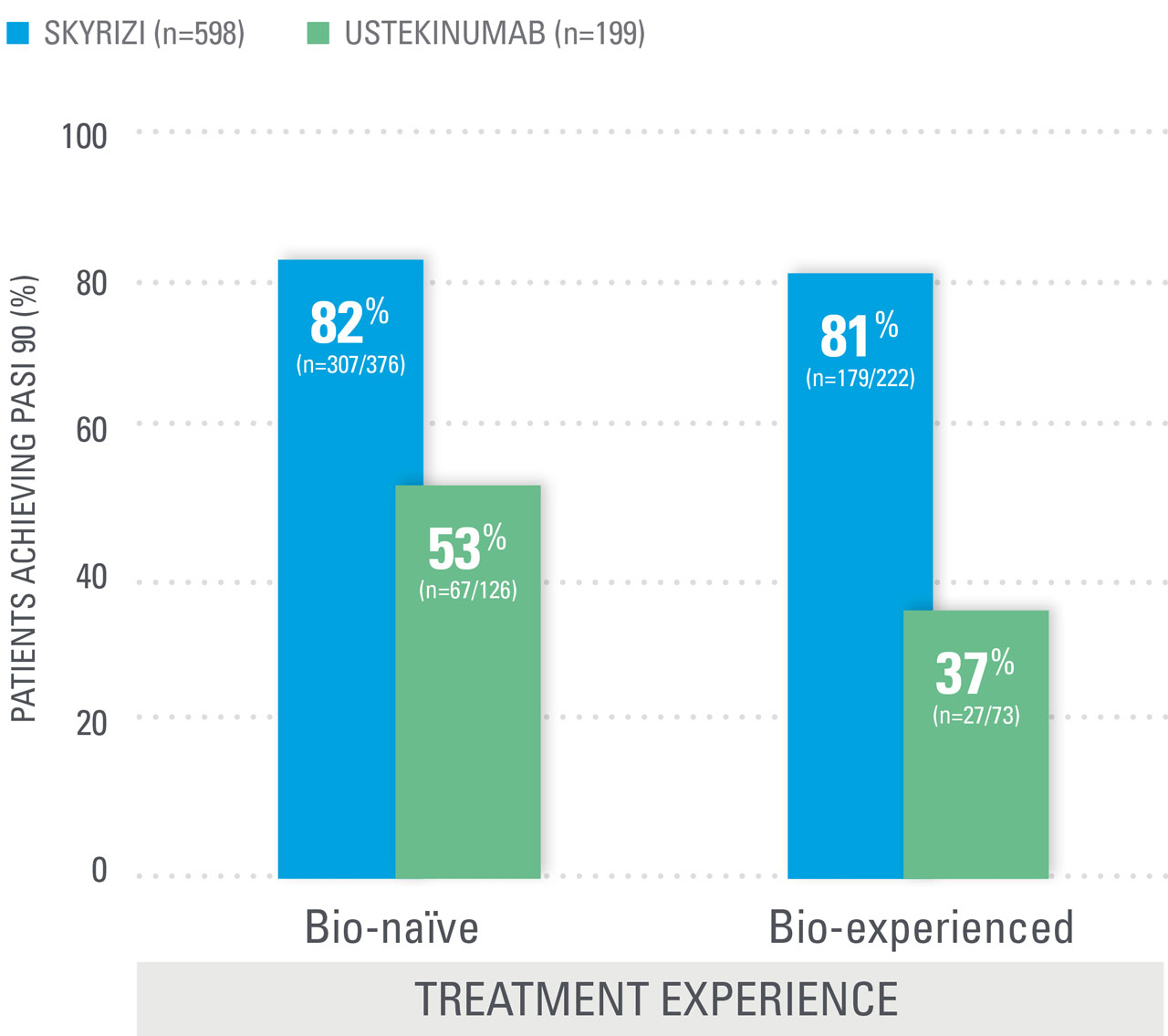
REGARDLESS OF BMI AND PsO TREATMENT EXPERIENCE
more SKYRIZI patients achieved PASI 90 at Week 52 than patients on ustekinumab12
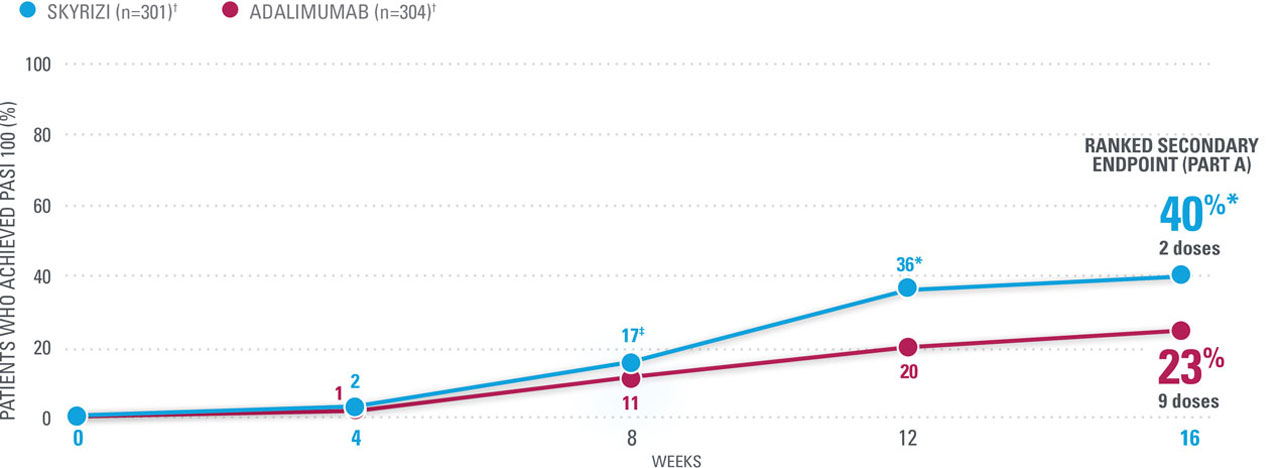
COMPLETE CLEARANCE in more patients compared to adalimumab
SUPERIOR AT WEEK 16: 40% OF SKYRIZI PATIENTS ACHIEVED PASI 100 VS 23% ADALIMUMAB (NRI)1,16*
In patients with a response of PASI ≥50 to <90 after 16 weeks of adalimumab treatment
SUPERIOR AT WEEK 44: 40% MORE PATIENTS ACHIEVED PASI 100 AFTER SWITCHING TO SKYRIZI THAN THOSE WHO STAYED ON ADALIMUMAB (NRI)1,16*
| * | P<0.0001 vs adalimumab. |
| † | SKYRIZI doses denoted in blue: Patients were stratified by weight (≤100 kg vs >100 kg) and prior TNF inhibitor exposure (no vs yes) and randomized 1:1 to receive 150 mg SKYRIZI (Weeks 0, 4, and 16) or adalimumab (80 mg at Week 0, 40 mg every other week [EOW]) from Week 1. |
| ‡ | P=0.0171 vs adalimumab; §P=0.0220 vs adalimumab; llP=0.0022 vs adalimumab; ¶P=0.0073 vs adalimumab; #P=0.0002 vs adalimumab |
| Adalimumab-treated patients achieving PASI 50 to <90 at Week 16 were stratified by weight and prior TNF inhibitor exposure and rerandomized 1:1 to either continue adalimumab EOW until Week 41 or switch to SKYRIZI (Weeks 16, 20, and 32). | |
| Inadequate or partial response in the IMMvent study was defined as PASI ≥50 to <90 at Week 16 in patients receiving adalimumab. |
IMMvent Phase 3 study design16
A 44-week, randomized comparative study vs adalimumab in patients with moderate to severe chronic plaque psoriasis (N=605)
Nothing more than 4 INJECTIONS PER YEAR after initiation doses for both PsO and PsA patients1*
NO DOSE ADJUSTMENT regardless of baseline characteristics, including BMI and weight1,11,12†
- SKYRIZI is dosed 150 mg (one 150-mg subcutaneous injection) at Week 0, Week 4, and every 12 weeks thereafter for adult patients with moderate to severe PsO or active PsA.1
- Low rate of injection site reactions at Week 16 (based on an analysis of 5 PsO clinical trials: SKYRIZI 1.5% vs placebo 1.0%)13
—In a long-term PsO analysis (up to 8.8 years), rates of injection site reactions were low for SKYRIZI patients (2.8 E/100 PY).14‡
Consideration should be given to discontinuing treatment in patients who have shown no response after 16 weeks of treatment. Some patients with initial partial response may subsequently improve with continued treatment beyond 16 weeks.
| * | Maintenance dosing (one 150-mg subcutaneous injection/dose) every 12 weeks following a starter dose at Week 0 and Week 4. If a dose is missed, the dose should be administered as soon as possible. Thereafter, dosing should be resumed at the regular scheduled time. |
| † | Risankizumab clearance and volume of distribution increase as body weight increases, which may result in reduced efficacy in subjects with high body weight (>130 kg). However, this observation is based on a limited number of subjects. |
| ‡ | Week 16 (5-study pool) and long-term (median duration of treatment 4.1 years [ranging from 81 days to 8.8 years] 20-study pool) represent different pools of patients with varying lengths of treatment exposure included in the long-term data set.14 |
SKYRIZI one injection per dose:
SAME EFFICACY AND SAFETY PROFILE
Same active ingredient | Demonstrated bioequivalence1
NOW EVEN SIMPLER WITH
SKYRIZI 150 mg bioequivalence data1
Bioequivalence was demonstrated between a single SKYRIZI 150-mg injection and two SKYRIZI 75-mg injections in a prefilled syringe. Bioeqivalence was also demonstrated between SKYRIZI 150 mg in a prefilled syringe and a prefilled pen.
REGARDLESS OF BMI AND PsO TREATMENT EXPERIENCE
more SKYRIZI patients achieved PASI 90 at Week 52 than patients on ustekinumab12
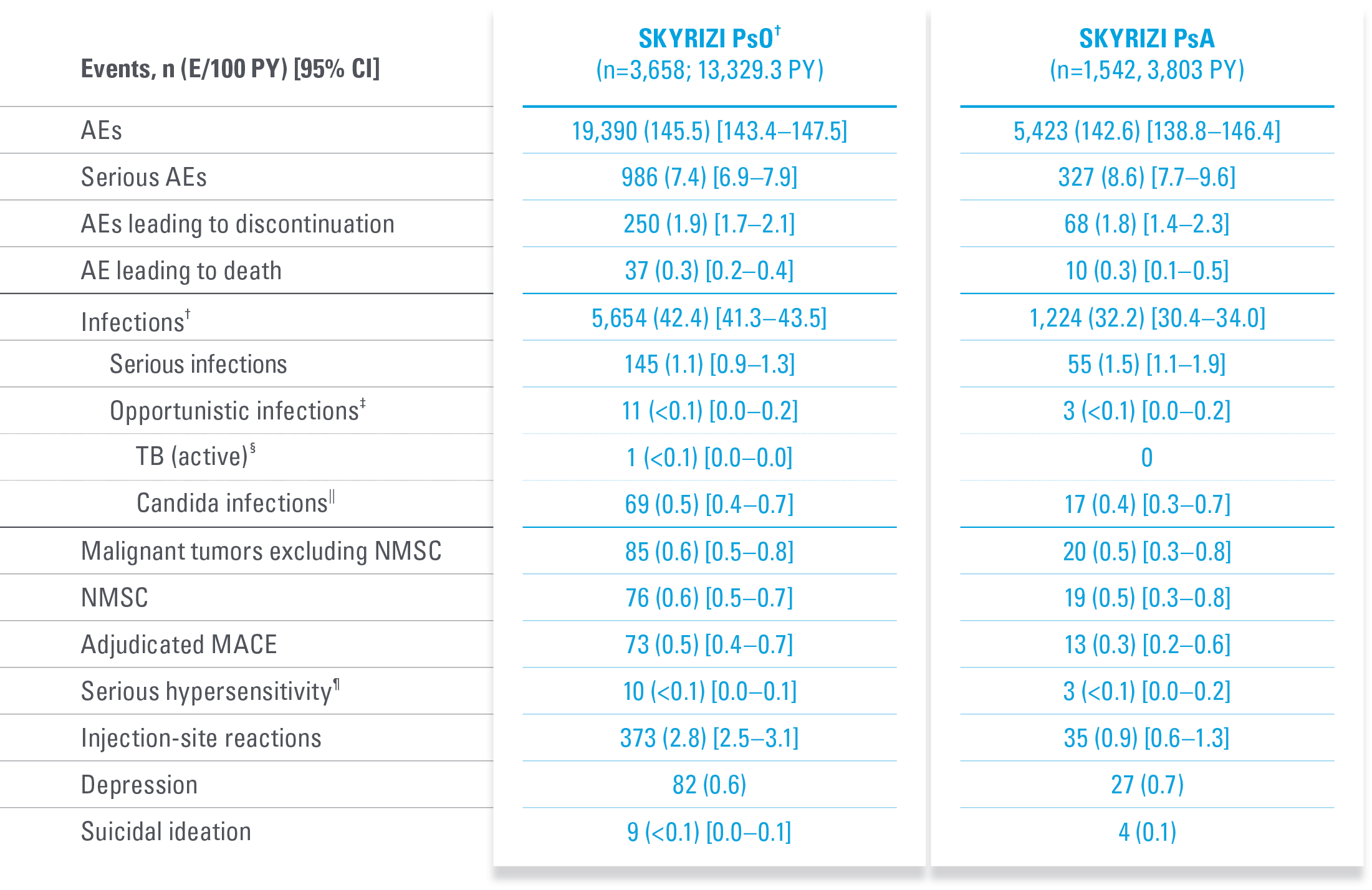
A FAVORABLE PsO SAFETY PROFILE1
No cases of active TB reported in controlled periods of PsO and PsA trials, inlcuding 31 IMMhance study patients with latent TB who did not receive prophylaxis1,18,20-22
Prior to and during SKYRIZI
treatment, evaluate and monitor
patients for TB. Consider anti-TB
therapy prior to initiating
SKYRIZI in patients with
history of latent or active TB.1
Safety profile in PsA consistent with safety profile observed in PsO1
| * | Integrated all-risankizumab safety data set from 20 completed or ongoing Phase 1-4 risankizumab clinical trials in plaque psoriasis (data cutoff March 25, 2023). Median duration of treatment was 4.1 years (ranging from 81 days to 8.8 years).15 |
Important contextual information1
SKRYIZI is contraindicated in patients with clinically important active infections (e.g., active tuberculosis).
Tuberculosis: Prior to initiating treatment with SKYRIZI, patients should be evaluated for tuberculosis (TB) infection. Patients receiving SKYRIZI should be monitored for signs and symptoms of active TB. Anti-TB therapy should be considered prior to initiating SKYRIZI in patients with a past history of latent or active TB in whom an adequate course of treatment cannot be confirmed.
Lab monitoring: SKYRIZI may increase the risk of infection. In patients with a chronic infection, a history of recurrent infection, or known risk factors for infection, SKYRIZI should be used with caution.
Treatment with SKYRIZI should not be initiated in patients with any clinically important active infection until the infection resolves or is adequately treated. Patients treated with SKYRIZI should be instructed to seek medical advice if signs or symptoms of clinically important chronic or acute infection occur. If a patient develops such an infection or is not responding to standard therapy for the infection, the patient should be closely monitored and SKYRIZI should not be administered until the infection resolves.
| * | UltIMMa: One non–treatment-emergent death of unknown cause on study Day 189 that occurred 161 days after the last dose of study drug. |
| † | IMMvent: One patient with acute myocardial infarction on study Day 73 (event was not considered to be study drug–related by investigator). |
| ‡ | IMMhance: One patient with stroke reported as ischemic stroke on study Day 95. |
| § | IMMhance: One patient with esophageal carcinoma reported on study Day 16, with patient experiencing 40 lbs weight loss six months prior to study participation; one patient with malignant melanoma in situ reported on study Day 102, study drug was not interrupted; one patient with a cutaneous squamous cell carcinoma reported on study Day 89, study drug was not interrupted. |
A safety profile similar to ustekinumab in PsO through Week 52 during RCTs:18
- UltIMMa-1—Any AE: SKYRIZI 61.3% (n=182/297) vs ustekinumab 66.7% (n=66/99); Serious AEs: SKYRIZI 5.4% (n=16/297) vs ustekinumab 4.0% (n=4/99); Infections: SKYRIZI 37.7% (n=112/297) vs ustekinumab 41.4% (n=41/99)
- UltIMMa-2—Any AE: SKYRIZI 55.7% (n=162/291) vs ustekinumab 74.5% (n=70/94); Serious AEs: SKYRIZI 4.5% (n=13/291) vs ustekinumab 4.3% (n=4/94); Infections: SKYRIZI 34.7% (n=101/291) vs ustekinumab 48.9% (n=46/94)
Through Week 52, the frequency of the adverse reactions was similar to the safety profile observed during the first 16 weeks of treatment. Through Week 52, the exposure-adjusted rates of serious adverse events per 100 subject-years were 9.4 for subjects treated with SKYRIZI and 10.9 for those treated with ustekinumab. For those subjects exposed to a maximum of 77 weeks of SKYRIZI, no new adverse reactions were identified compared to the first 16 weeks of treatment.1
A FAVORABLE SAFETY PROFILE EVALUATED UP TO 8.8 YEARS IN PsO WITH PsA DATA UP TO 4 YEARS15,17*
Treatment-emergent AEs from an integrated analysis of PsO and PsA clinical trials15
SKYRIZI warnings and precautions include infections, tuberculosis, and immunizations.1
Additional study details15
- Nasopharyngitis and upper respiratory infection were the most common infections in patients with psoriasis and patients with psoriatic arthritis.
- Excluding COVID-related infections, the most common serious infections (sepsis, pneumonia, and cellulitis) were similar in psoriasis and psoriatic arthritis.
- The rates of serious infections excluding COVID-related infections with SKYRIZI were within the reference rates for serious infections reported for psoriasis (PSOLAR: 0.93–2.91 E/100 PY and psoriatic arthritis (PSOLAR: 1.00–3.01 E/100 PY).
- Rates of opportunistic infections excluding tuberculosis and herpes zoster (both <0.1 E/100 PY) and herpes zoster (0.5 and 0.3 E/100 PY) were comparable for psoriasis and psoriatic arthritis, respectively.
| * | Long-term safety was evaluated using integrated all-risankizumab safety data sets (data cutoff March 25, 2023) from 20 Phase 1–4 clinical trials in PsO and 4 Phase 2 and 3 trials in PsA. Median (range) of treatment duration for PsO was 4.1 years (81 days to 8.8 years) and for PsA was 2.8 years (84 days to 4.0 years). For all patients who received ≥1 dose of risankizumab (all administered doses, 18 mg to 180 mg), AEs and AEs of special interest were assessed and recorded through the end of exposure (last dose to first dose + 5 geometric-mean half-lives [20 weeks]). |
| † | Excluding COVID-related infections. |
| ‡ | Excluding tuberculosis and herpes zoster. |
| § | One case of active tuberculosis was reported from Taiwan. The patient in a long-term open-label psoriasis study had latent tuberculosis diagnosed at screening of the feeder study and received isoniazid prophylaxis. He presented with a cough for 4 years after study initiation and was diagnosed based on positive sputum and chest X-ray (diagnostic results such as PCR/culture not provided). |
| || | By system organ class. |
| ¶ | Reported events: eczema (2), Stevens-Johnson syndrome (2), urticaria (2), angioedema (1), drug hypersensitivity (1), erythema multiforme (1), hypersensitivity (1). |
Measurements were taken at each time point prior to administration of the next dose.
Patient depicted was a participant in the UltIMMa-2 pivotal trial undergoing continuous treatment with SKYRIZI for moderate to severe plaque psoriasis.1,8
DoF ABVRRTI67530
ACR=American College of Rheumatology; ADA=adalimumab; AE=adverse events; bio-IR=inadequate response to a biologic; BMI=body mass index; CI=confidence interval; csDMARD-IR=inadequate response to a conventional synthetic DMARD; DLQI=Dermatology Life Quality Index; DMARD=disease-modifying antirheumatic drug; E=event; IBD=inflammatory bowel disease; IL=interleukin; LDI=Leeds Dactylitis Index; LEI=Leeds Enthesitis Index; MACE=major adverse cardiovascular event; MTX=methotrexate; NMSC=nonmelanoma skin cancer; NRI=nonresponder imputation; OC=observed case; OLE=open-label extension; PASI=Psoriasis Area and Severity Index; PBO=placebo; PsA=psoriatic arthritis; PsO=psoriasis; PSS=psoriasis symptom scale; PY=patient-year; RCT=randomized controlled trial; sPGA=static Physician’s Global Assessment; TB=tuberculosis; TEAE=treatment-emergent adverse event; TNF=tumor necrosis factor; UST=ustekinumab.
EU Indications and Important Safety Information for SKYRIZI
INDICATIONS1
SKYRIZI (risankizumab) is indicated for the treatment of moderate to severe plaque psoriasis in adults who are candidates for systemic therapy.
SKYRIZI (risankizumab), alone or in combination with methotrexate (MTX), is indicated for the treatment of active psoriatic arthritis in adults who have had an inadequate response or who have been intolerant to one or more disease-modifying antirheumatic drugs (DMARDs).
SKYRIZI is indicated for the treatment of adult patients with m oderately to severely active Crohn’s disease who have had an inadequate response to, lost response to, or were intolerant to conventional therapy or a biologic therapy.
IMPORTANT SAFETY INFORMATION1
Risankizumab is contraindicated in patients hypersensitive to the active substance or to any of the excipients, and in patients with clinically important active infections (e.g. active tuberculosis). Risankizumab may increase the risk of infection. In patients with a chronic infection, a history of recurrent infection, or known risk factors for infection, risankizumab should be used with caution. Treatment with risankizumab should not be initiated in patients with any clinically important active infection until the infection resolves or is adequately treated.
Patients treated with risankizumab should be instructed to seek medical advice if signs or symptoms of clinically important chronic or acute infection occur. If a patient develops such an infection or is not responding to standard therapy for the infection, the patient should be closely monitored and risankizumab should not be administered until the infection resolves.
Prior to initiating treatment with risankizumab, patients should be evaluated for tuberculosis (TB) infection. Patients receiving risankizumab should be monitored for signs and symptoms of active TB. Anti-TB therapy should be considered prior to initiating risankizumab in patients with a past history of latent or active TB in whom an adequate course of treatment cannot be confirmed.
Prior to initiating therapy with risankizumab, completion of all appropriate immunisations should be considered according to current immunisation guidelines. If a patient has received live vaccination (viral or bacterial), it is recommended to wait at least 4 weeks prior to starting treatment with risankizumab. Patients treated with risankizumab should not receive live vaccines during treatment and for at least 21 weeks after treatment.
If a serious hypersensitivity reaction occurs, administration of risankizumab should be discontinued immediately and appropriate therapy initiated.
The most frequently reported adverse reactions were upper respi ratory infections (from 13% in psoriasis to 15.6% in Crohn’ s disease). Commonly (≥ 1/100 to < 1/10) reported adverse reactions include d tinea infections, headache, pruritus, fatigue, and injection site reactions.
This is not a complete summary of all safety information. Please see the SmPC for complete prescribing information.
References
- SKYRIZI [Summary of Product Characteristics]. AbbVie Ltd; March 2024.
- Puig L. PASI90 response: the new standard in therapeutic efficacy for psoriasis. J Eur Acad Dermatol Venereol. 2015;29(4):645-648. doi:10.1111/jdv.12817
- Strober B, Papp KA, Lebwohl M, et al. Clinical meaningfulness of complete skin clearance in psoriasis. J Am Acad Dermatol. 2016;75(1):77-82.e7. doi:10.1016/j.jaad.2016.03.026
- Gooderham MJ, Papp KA, Lynde CW. Shifting the focus – the primary role of IL-23 in psoriasis and other inflammatory disorders. J Eur Acad Derm Venereol. 2018;32(7):1111-1119. doi:10.1111/jdv.14868
- Gaffen SL, Jain R, Garg AV, Cua DJ. The IL-23-IL-17 immune axis: from mechanisms to therapeutic testing. Nature Rev Immunol. 2014;14(9):585-600. doi:10.1038/nri3707
- Girolomoni G, Strohal R, Puig L, et al. The role of IL-23 and the IL-23/TH17 immune axis in the pathogenesis and treatment of psoriasis. J Eur Acad Dermatol Venereol. 2017;31(10):1616-1626. doi:10.1111/jdv.14433
- Lynde CW, Poulin Y, Vender R, Bourcier M, Khalil S. Interleukin 17A: toward a new understanding of psoriasis pathogenesis. J Am Acad Dermatol. 2014;71(1):141-150. doi:10.1016/j.jaad.2013.12.036
- Gordon KB, Strober B, Lebwohl M, et al. Efficacy and safety of risankizumab in moderate-to-severe plaque psoriasis (UltIMMa-1 and UltIMMa-2): results from two double-blind, randomised, placebo-controlled and ustekinumab-controlled phase 3 trials. Lancet. 2018;392(10148):650-661. doi:10.1016/S0140-6736(18)31713-6
- Gordon KB, Strober B, Lebwohl M, et al. Supplement to: Efficacy and safety of risankizumab in moderate-to-severe plaque psoriasis (UltIMMa-1 and UltIMMa-2): results from two double-blind, randomised, placebo-controlled and ustekinumab-controlled phase 3 trials. Lancet. 2018;392(10148):650-661. doi:10.1016/S0140-6736(18)31713-6
- Data on File, AbbVie Inc. ABVRRTI67791.
- Leonardi C, Gordon K, Longcore M, Gu Y, Puig L. Weight-based analysis of psoriasis area and severity index improvement at 52 weeks of risankizumab or ustekinumab treatment: an integrated analysis of patients with moderate-to-severe plaque psoriasis. Presented at: 24th World Congress of Dermatology (WCD); June 10–15, 2019; Milan, Italy. Poster 5248.
- Strober B, Menter A, Leonardi C, et al. Efficacy of risankizumab in patients with moderate-to-severe plaque psoriasis by baseline demographics, disease characteristics and prior biologic therapy: an integrated analysis of the phase III UltIMMa-1 and UltIMMa-2 studies. J Eur Acad Dermatol Venereol. 2020;34(12):2830-2838. doi:10.1111/jdv.16521
- Leonardi C, Bachelez H, Wu JJ, et al. Safety of risankizumab in patients with moderate to severe psoriasis: analysis of pooled short-term and long-term clinical trial data. Poster presented at: 24th World Congress of Dermatology (WCD); June 10–15, 2019; Milan, Italy. Poster 3591.
- Gordon KB, Blauvelt A, Coates L, et al. Risankizumab Long-Term Safety in Patients With Psoriatic Disease: Integrated Analyses of Data From Psoriasis and Psoriatic Arthritis Clinical Trials Poster presented at: 2022 European Academy of Dermatology and Venereology (EADV) Virtual Congress; September 7–10, 2022. Poster 1607.
- Blauvelt A, Gordon KB, Lee P, et al. Efficacy, safety, usability, and acceptability of risankizumab 150 mg formulation administered by prefilled syringe or by an autoinjector for moderate to severe plaque psoriasis. J Dermatolog Treat. 2021;1-9. doi:10.1080/09546634.2021.1914812
- Reich K, Gooderham M, Thaçi D, et al. Risankizumab compared with adalimumab in patients with moderate-to-severe plaque psoriasis (IMMvent): a randomised, double-blind, active-comparator-controlled phase 3 trial. Lancet. 2019;394(10198):576-586. doi:10.1016/S0140-6736(19)30952-3
- Blauvelt A, Papp KA, Gooderham M, et al. Efficacy and safety of risankizumab, an IL-23 inhibitor, in patients with moderate-to-severe chronic plaque psoriasis: 16-week results from the phase 3 IMMhance trial. Paper presented at: Psoriasis: From Gene to Clinic Meeting, November 30–December 3, 2017; London, United Kingdom.
- Langley RG, Blauvelt A, Gooderham M, et al. Efficacy and safety of continuous Q12W risankizumab versus treatment withdrawal: results from the phase 3 IMMhance trial. Poster presented at: 2019 American Academy of Dermatology (AAD) Annual Meeting; March 1–5, 2019; Washington, DC. Poster 10093.
- Gordon KA, Lebwohl M, Papp KA, et al. Long-term safety of risankizumab from 17 clinical trials in patients with moderate-to-severe plaque psoriasis. Br J Dermatol. 2021;186(3):466-475. doi: 10.1111/bjd.20818
- Warren RB, Blauvelt A, Poulin Y, et al. Efficacy and safety of risankizumab vs. secukinumab in patients with moderate-to-severe plaque psoriasis (IMMerge): results from a phase III, randomized, open-label, efficacy-assessor-blinded clinical trial. Br J Dermatol. 2021;184(1):50-59. doi:10.1111/bjd.19341
- Data on File, AbbVie Inc. ABVRRTI67790.
- Papp K, Lebwohl MG, Puig L, et al. Long-term Safety and Efficacy of Risankizumab for the Treatment of Moderate-to-Severe Plaque Psoriasis: Interim Analysis From the LIMMitless Open-label Extension Trial Beyond 5.5 Years of Follow-up. Poster presented at: 2023 American Academy of Dermatology Annual Meeting (AAD 2023), March 17–21, New Orleans, LA, USA. Poster 43928.
- Data on File, AbbVie Inc. ABVRRTI70545.
- Strober B, Eyerich K, Hong HC, Zeng J, et al. Long-term efficacy and safety of switching from ustekinumab to risankizumab: results from the open-label extension LIMMitless. Poster presented at: 28th European Academy of Dermatology and Venereology (EADV) Congress; October 9–13, 2019; Madrid, Spain. Poster 1714.
- Strober B, Armstrong A, Rubant S, et al. Switching to risankizumab from ustekinumab or adalimumab in plaque psoriasis patients improves PASI and DLQI outcomes for sub-optimal responders. J Dermatolog Treat. 2022;1-7. doi:10.1080/09546634.2022.2095328
- Risankizumab versus secukinumab for subjects with moderate to severe plaque psoriasis. ClinicalTrials.gov identifier: NCT03478787. Updated July 13, 2021. Accessed June 7, 2023. https://clinicaltrials.gov/ct2/show/NCT03478787
- HUMIRA [Summary of Product Characteristics]. AbbVie Deutschland GmbH & Co. KG; October 2022.