This page and associated chart pop-ups should be unbranded based on disease presentation. Remove elements of branding color, brand logo, and name. Refer to your local country rules and regulations on disease presentation accordingly when presenting Unmet Need
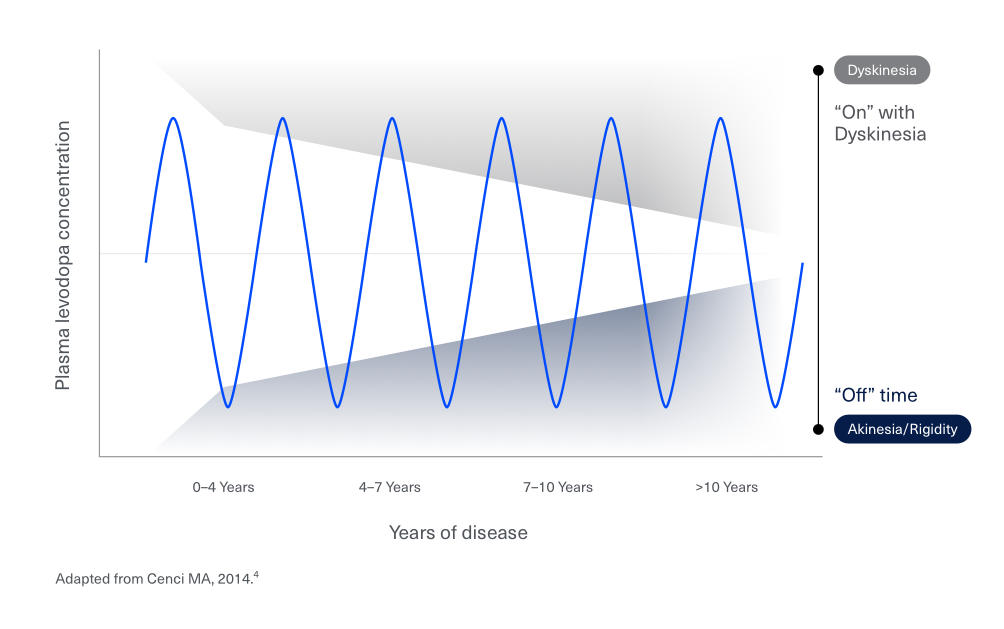
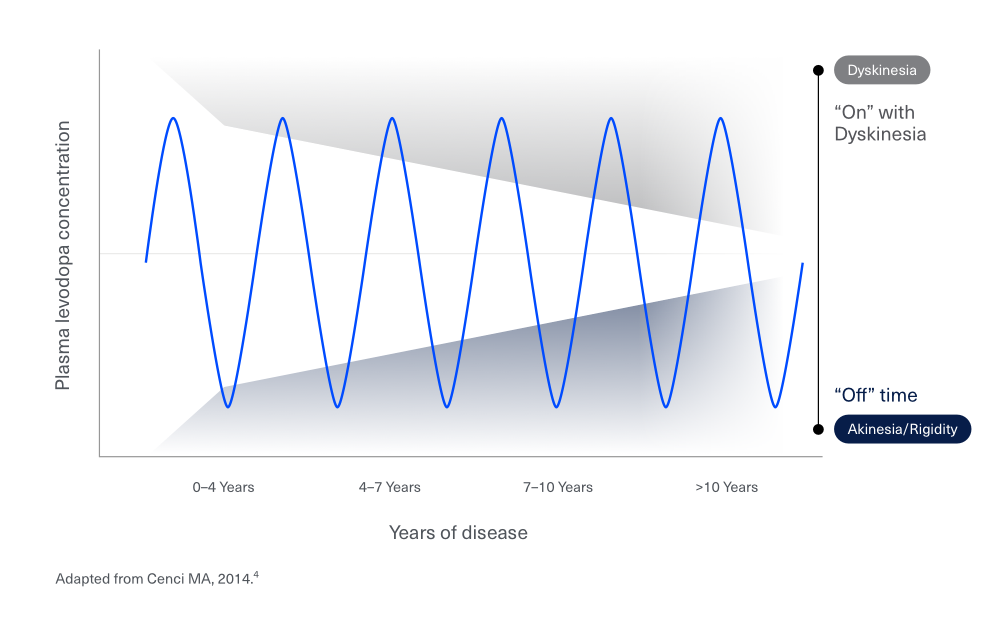
Historically, levodopa-based therapy has been the gold standard of PD treatment, but as patients’ therapeutic window narrows with disease progression, the benefits of oral levodopa-based therapy diminish.1,2
For the patient, this results in:1
- Susceptibility to more “On” time with dyskinesia
- An increase in “Off” time
- Diminished health-related quality of life
Note to affiliate: In the sample size of the PREDICT study indicated in the footnote (n=43/54), 43 is the sum of patients in the Hoehn and Yahr stages 3 and 4 (35 and 8, respectively).
*In the PREDICT study, 80% of patients in Hoehn and Yahr stage 3 or 4 who were being treated with oral levodopa (n=43/54) continued to take >5 oral levodopa units per day, even if most of them spent >50% of daily time in the “Off” state, with poor QoL in 65% of the patients in SOC and 41% of their caregivers, in addition to poor QoL reported by the treating physician.3
As PD progresses, the majority of patients may use three or more daily doses of PD medications at different times of the day5,6
HIGH PILL BURDEN AND COMPLEX REGIMENS ARE ASSOCIATED WITH:5,7
Patients’ and their care partners’ daily lives and activities, such as spending time with family, mealtimes, and going to the grocery store are dictated by unpredictable symptoms and medication schedules.6
FOR THE PATIENT THIS RESULTS IN:6
During waking hours, patients with PD may feel distress due to unpredictability of “Off” times, resulting in:1
- Insecurity about completing tasks or meeting social obligations due to unpredictability of “Off” times
- Increased sensitivity to events out of their control such as stress and variation in meals and mealtimes
Sleep disturbances are also common in patients with PD8
>50% OF PD PATIENTS report insomnia and about 2/3rds experience problems with sleep and ~60% OF PD PATIENTS report experiencing morning askinesia.8,9
REFERENCES
- Lundqvist C. Continuous levodopa for advanced Parkinson’s disease. Neuropsychiatr Dis Treat. 2007;3(3):335-348.
- Tambasco N, Romoli M, Calabresi P. Levodopa in Parkinson’s disease: current status and future developments. Curr Neuropharmacol. 2018;16(8):1239-1252.
- Tessitore A, Morano P, Modugno N, et al. Caregiver burden and its related factors in advanced Parkinson’s disease: data from the PREDICT study. J Neurol. 2018;265:1124-1137.
- Cenci MA. Presynaptic mechanisms of L-DOPA-induced dyskinesia: the findings, the debate, and the therapeutic implications. Front Neurol. 2014;5(242):1-15.
- Straka I, et al. Adherence to Pharmacotherapy in Patients With Parkinson's Disease Taking Three and More Daily Doses of Medication. Front Neurol. 2019;10:799.
- Tan QY, et al. The Experiences of Treatment Burden in People with Parkinson's Disease and Their Caregivers: A Systematic Review of Qualitative Studies. J Parkinsons Dis. 2021;11(4):1597-1617.
- Soileau MJ, et al. Comparative Effectiveness of Carbidopa-Levodopa Enteral Suspension and Deep Brain Stimulation on Parkinson's Disease-Related Pill Burden Reduction in Advanced Parkinson's Disease: A Retrospective Real-World Cohort Study. Neurol Ther. 2022 Jun;11(2):851-861.
- Gjerstad MD, Wentzel-Larsen T, Aarsland D, Larsen JP. Insomnia in Parkinson’s disease: frequency and progression over time. J Neurol Neurosurg Psychiatry. 2007;78:476-479.
- Chapuis S, Ouchchane L, Metz O, Gerbaud L, Durif F. Impact of the motor complications of Parkinson's disease on the quality of life. Mov Disord. 2005;20:224e30.