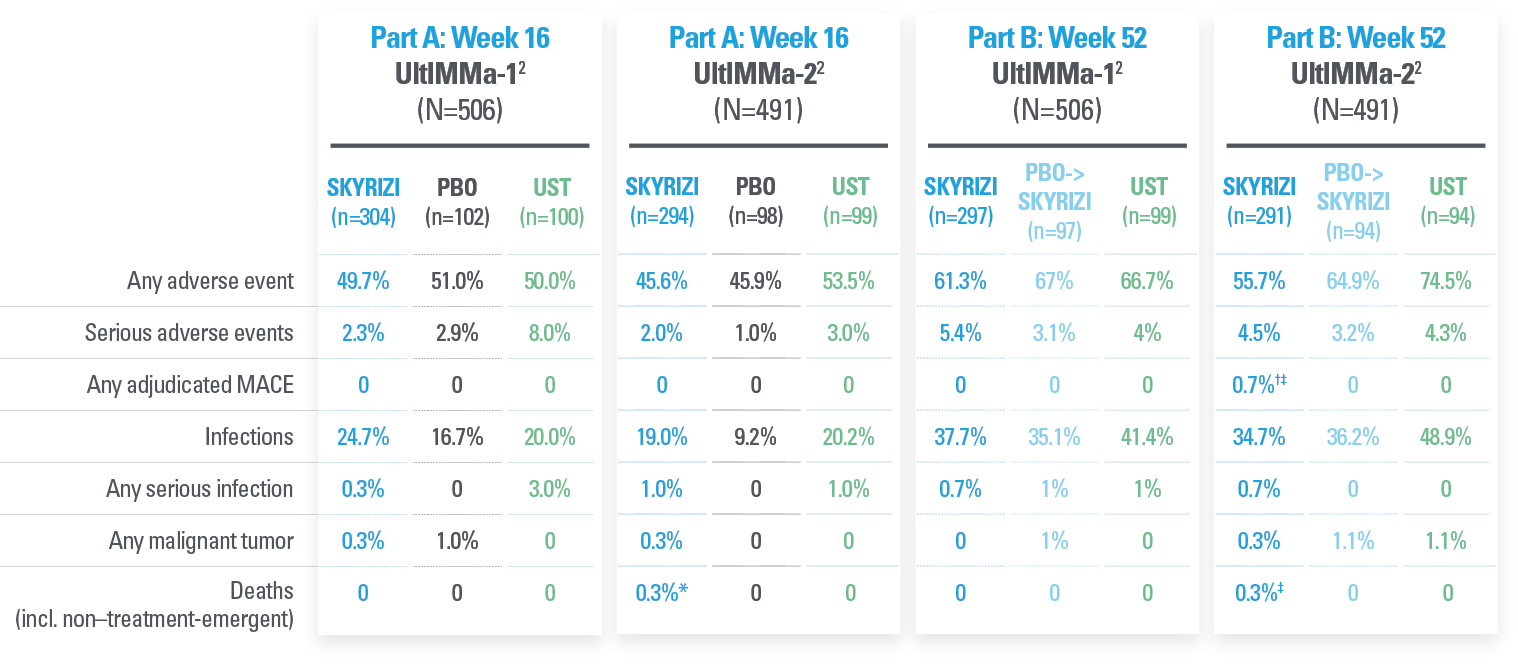
| * | Nothing on the skin: Defined as achievement of 75% PASI 90 and ≥84% sPGA 0/1 at Week 16 and achievement of ≥56% PASI 100 and sPGA 0 at Week 52 in UltIMMa-1 and UltIMMa-2.4 Please see full contextual information. |
SUPERIORITY DATA vs
4 AGENTS WITH 4 DIFFERENT MOAs1,2,5-7
Ustekinumab
IL-12/23i
UltIMMa-21,2
Phase 3 trial
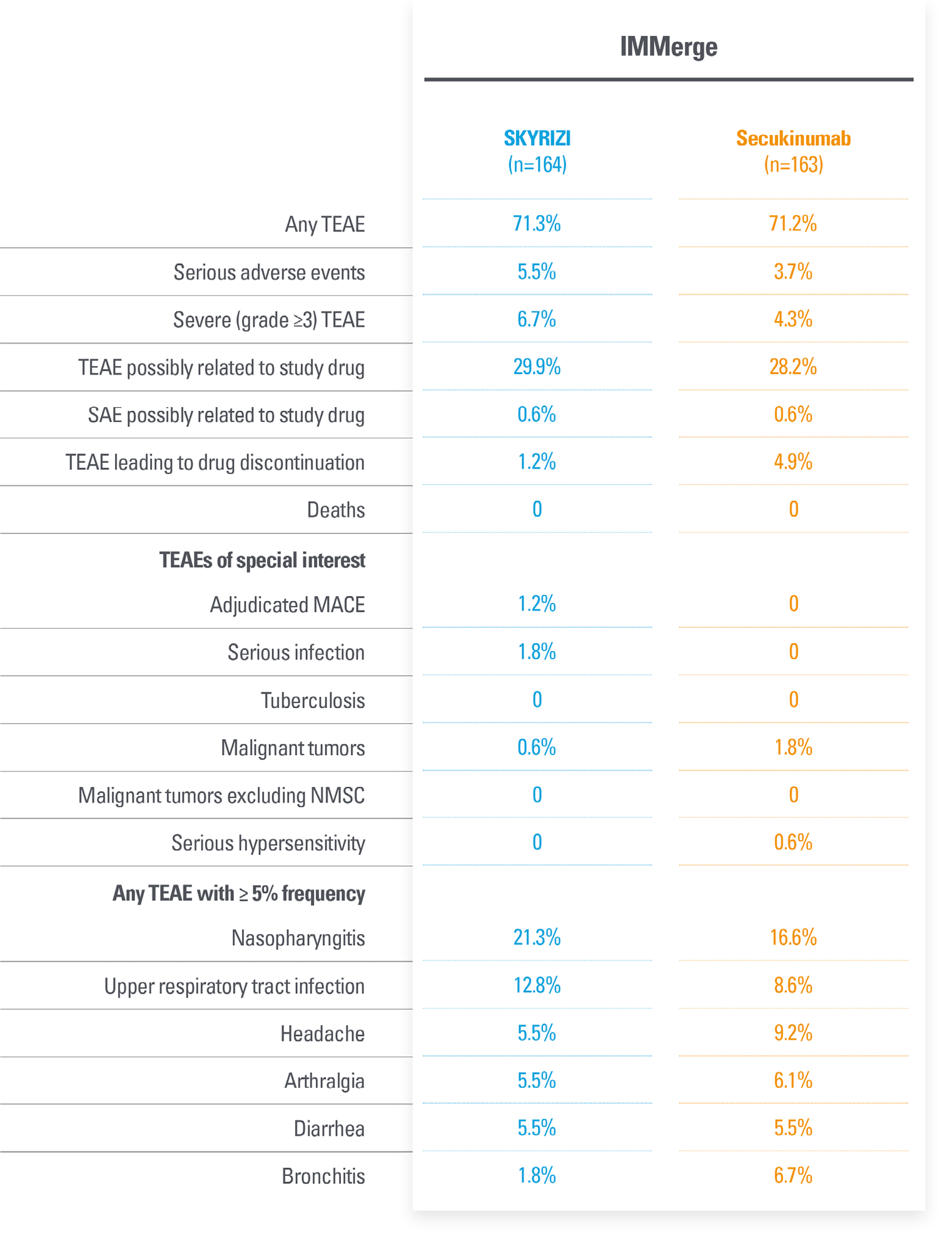
Secukinumab
IL-17i
IMMerge5
Phase 3b trial
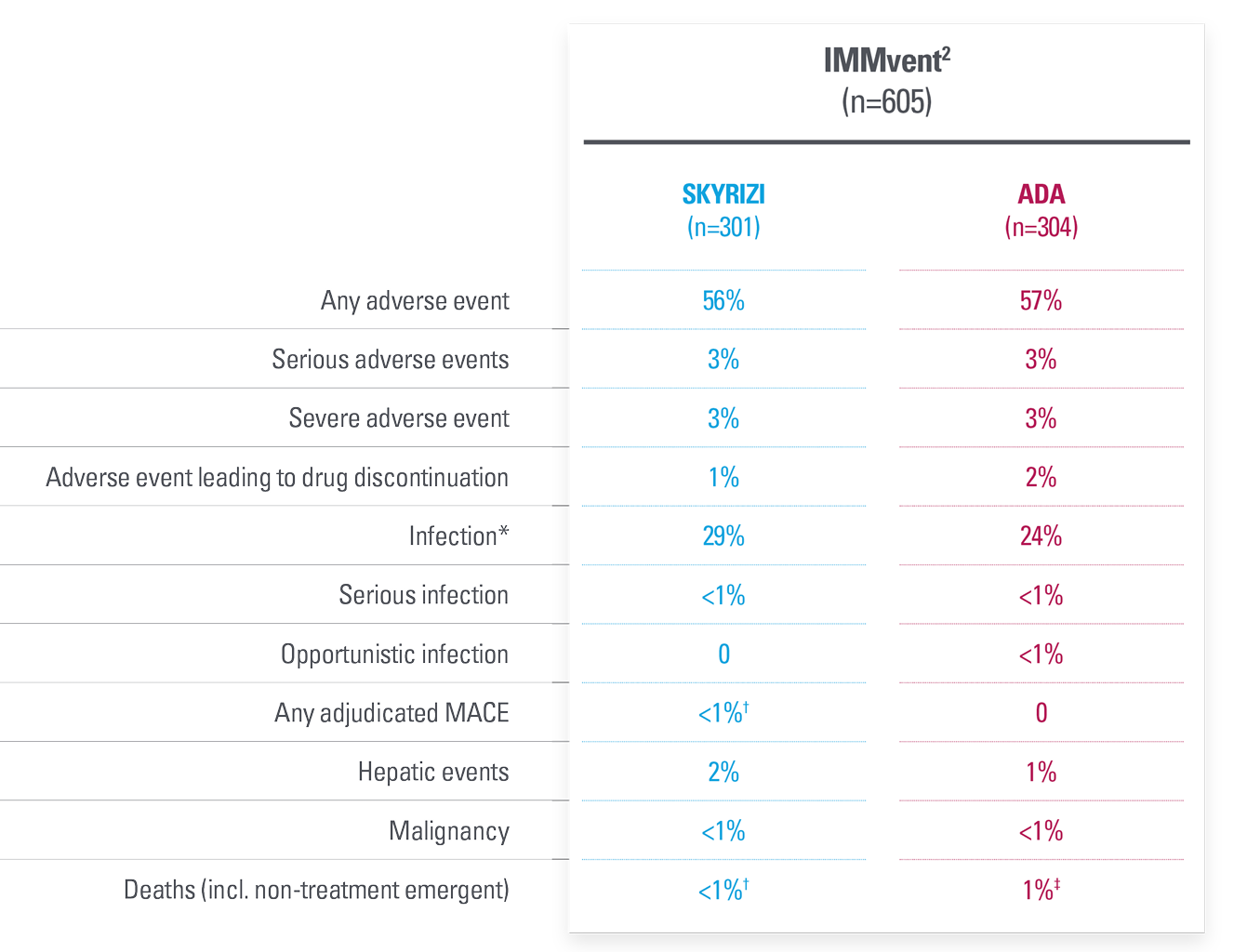
Adalimumab
TNFi
IMMvent6
Phase 3 trial
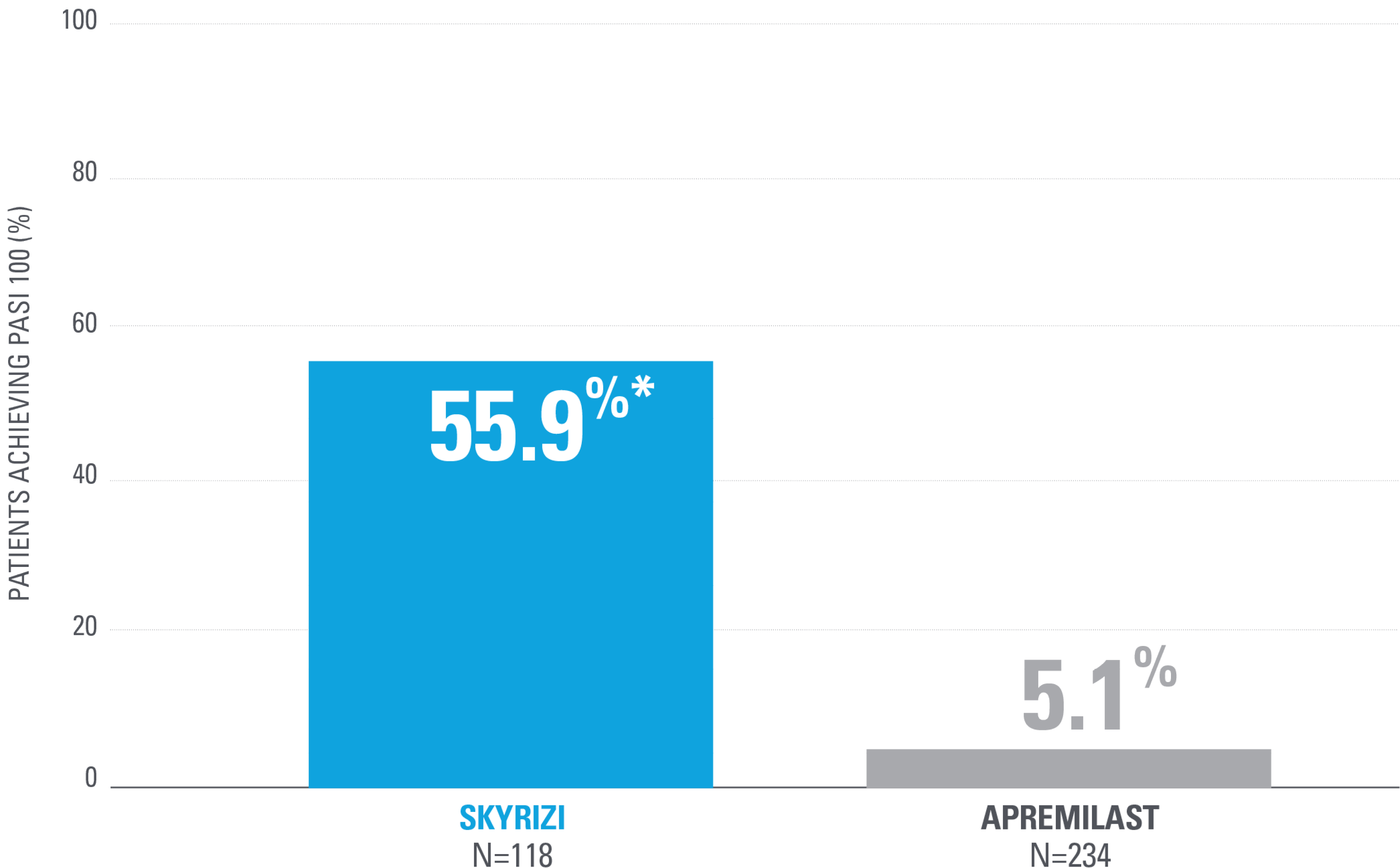
Apremilast
oral PDE4i
IMMpulse7
Phase 4 trial
Schedule a discussion with an AbbVie representative
[Affiliate To Update When They Localize]
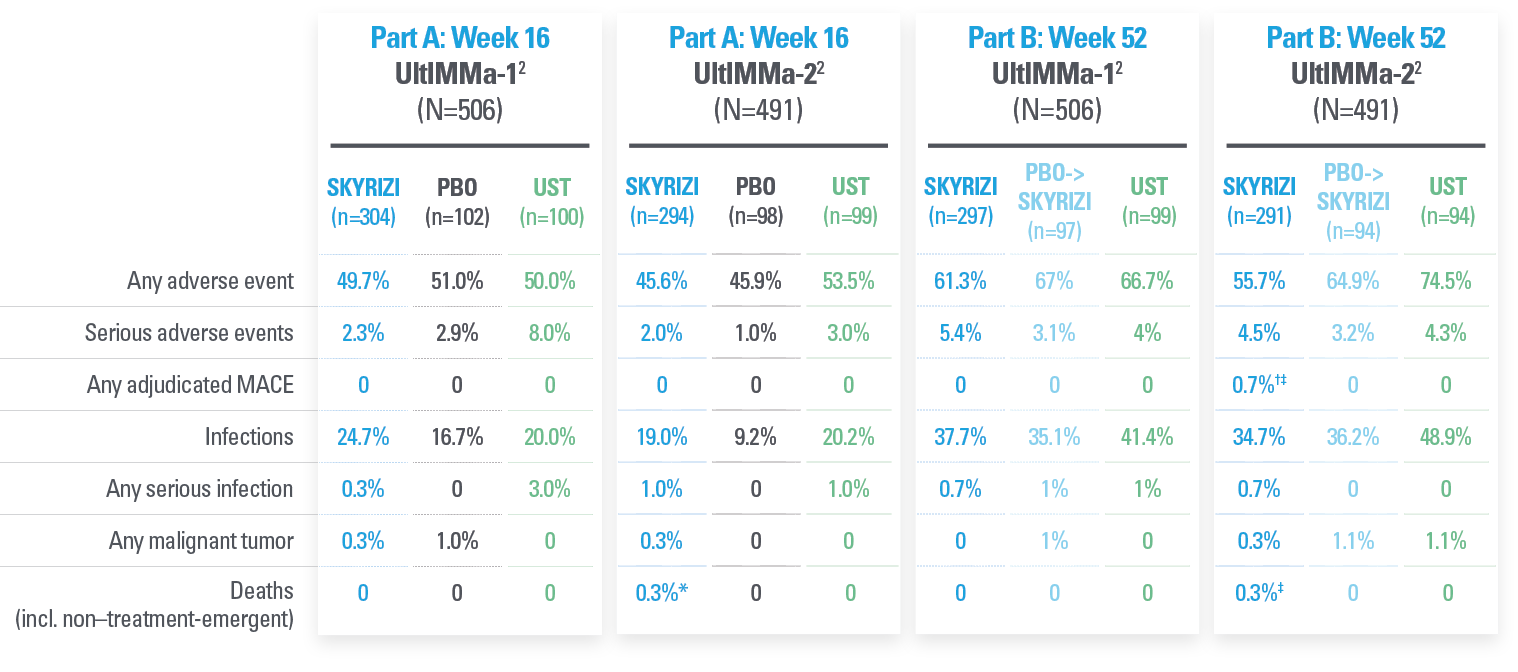
| * | SKYRIZI doses denoted in blue: Participants received 150 mg SKYRIZI at Week 0, Week 4, and every 12 weeks thereafter. Ustekinumab participants received either 45 mg or 90 mg (according to baseline weight) every 12 weeks after 2 starter doses at Week 0 and Week 4. | |
| † | P<0.0001 vs placebo.2 | |
| ‡ | P<0.0001 vs ustekinumab.2 | |
| Co-primary endpoint: 84% of patients achieved sPGA 0/1 at Week 16 with SKYRIZI vs 5% placebo (P<0.001).1 | ||
| Week 16 and 52 endpoints for PASI 90 were multiplicity controlled. All other data points shown were prespecified, nonranked endpoints that were not controlled for multiplicity. |
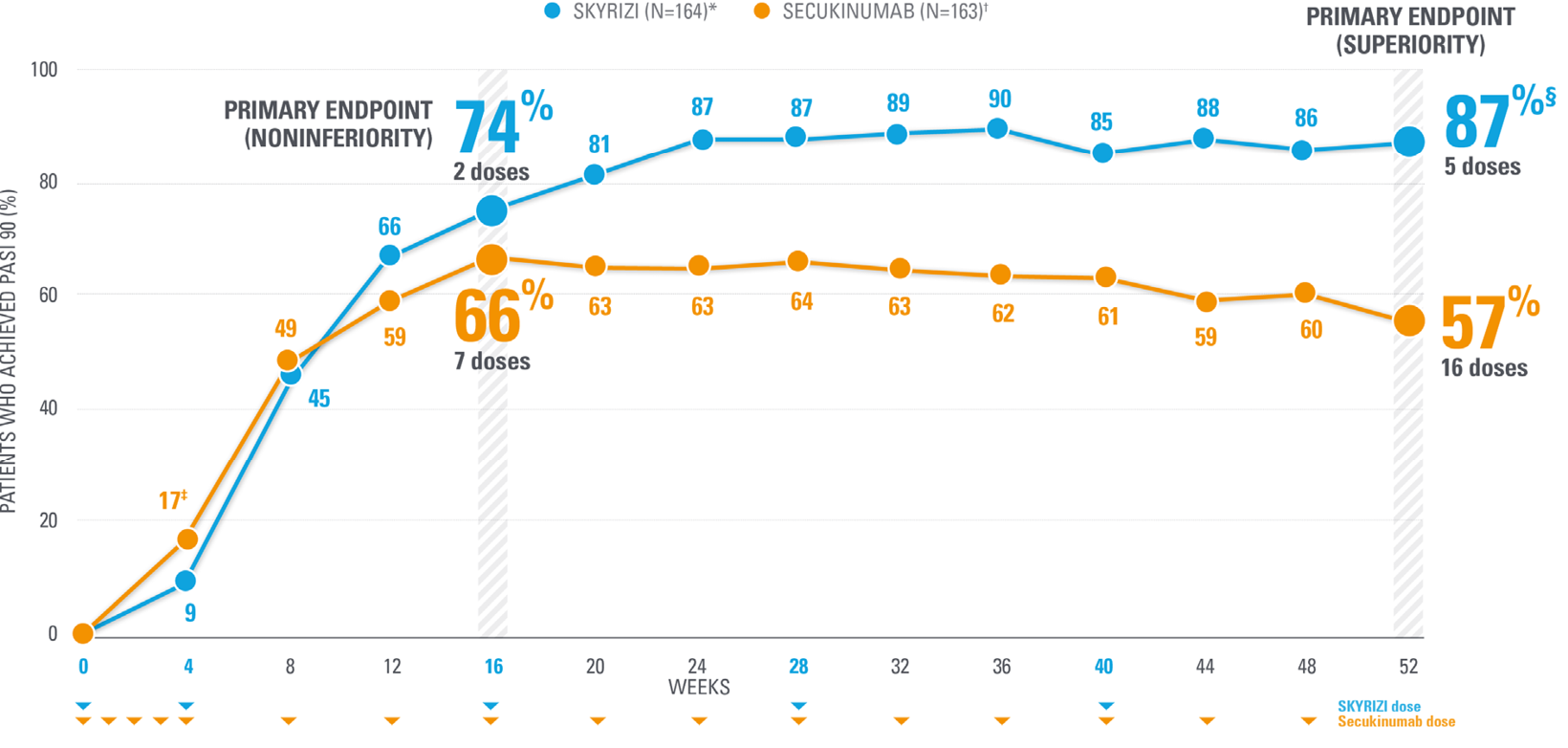
IMMerge: Phase 3b open-label, efficacy assessor-blinded trial in adult patients with moderate to severe PsO
SKYRIZI DEMONSTRATED SUPERIORITY AT ACHIEVING PASI 90 AT WEEK 52 vs SECUKINUMAB (IL-17i)
87% of SKYRIZI patients achieved PASI 90 (after 5 doses) vs 57% of patients taking secukinumab at Week 52 (16 doses) (NRI)5
| * | SKYRIZI doses denoted in blue: Participants received 150 mg SKYRIZI at Week 0, Week 4, and every 12 weeks thereafter. | |
| † | Secukinumab doses denoted in orange: Participants received 300 mg at Week 0, Week 2, Week 3, Week 4, and every 4 weeks thereafter. | |
| ‡ | P=0.039. | |
| § | P<0.001 vs secukinumab. | |
| Week 16 and 52 endpoints for PASI 90 were multiplicity-controlled. All other data points shown were prespecified nonranked endpoints that were not controlled for multiplicity |
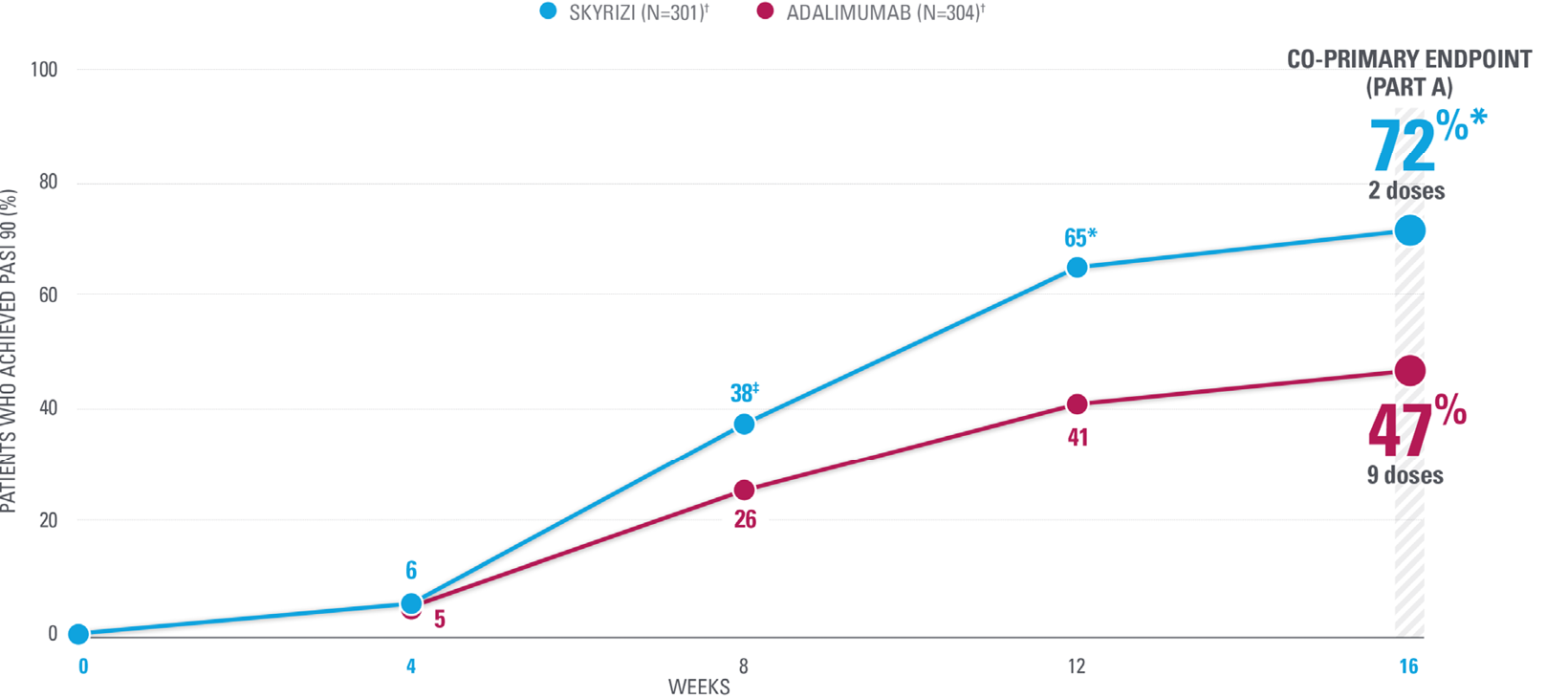
| Week 16 co-primary endpoint for PASI 90 was multiplicity controlled. All other data points shown were prespecified, nonranked endpoints that were not controlled for multiplicity. | |
| * | P<0.0001 vs adalimumab. |
| † | SKYRIZI doses denoted in blue: Patients were randomized 1:1 to receive 150 mg SKYRIZI (Weeks 0, 4, and 16) or adalimumab (80 mg at Week 0, 40 mg EOW) from Week 1. |
| ‡ | Nominal P=0.0012 vs adalimumab. |
| § | Nominal P<0.001 vs adalimumab. |
| Co-primary endpoint: 84% of patients achieved sPGA 0/1 at Week 16 with SKYRIZI vs 60% adalimumab (P<0.0001).6 |
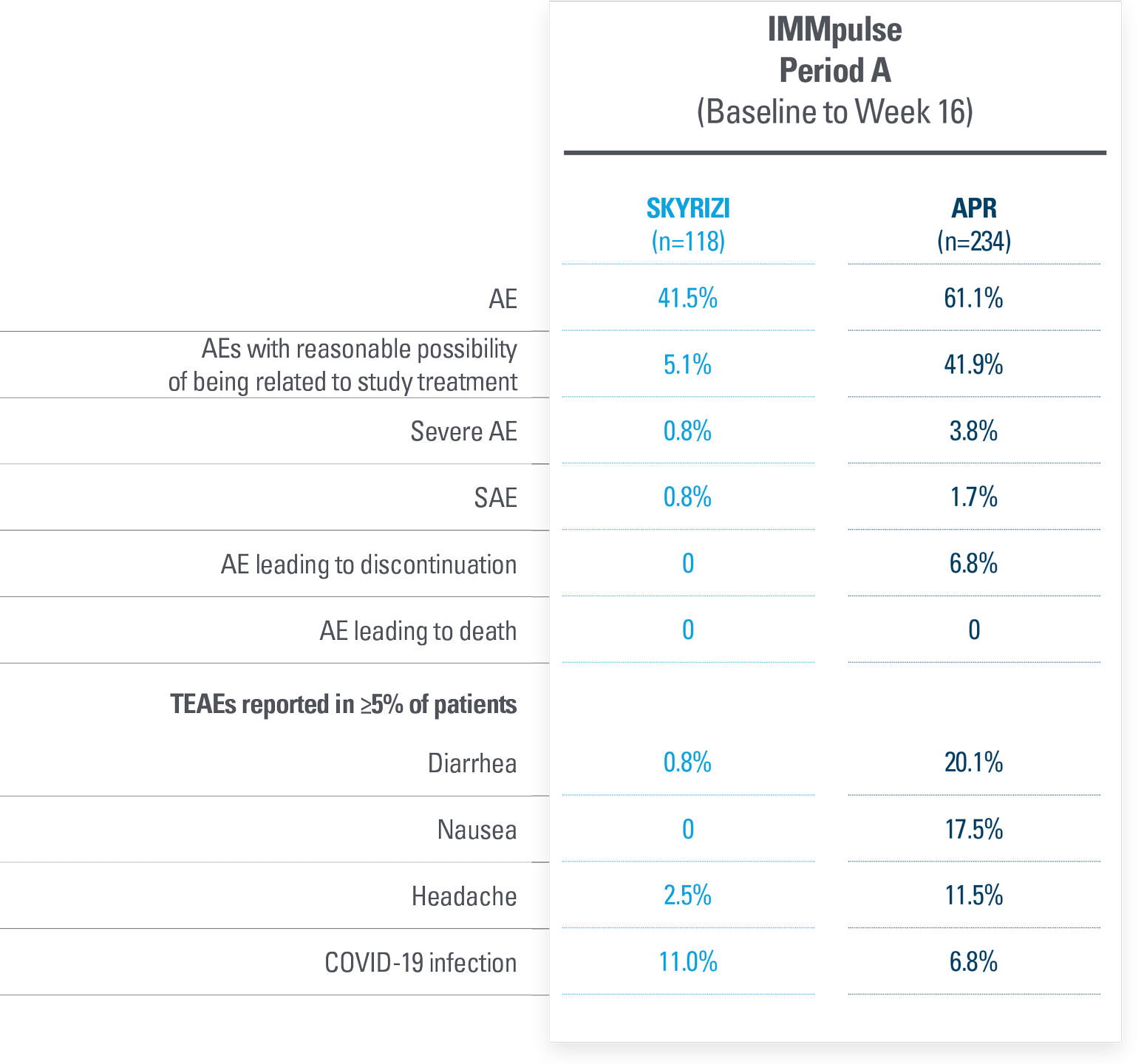
| Note to Affiliate: PASI 90 was 55.9% for SKY and 5.1% for APR at Week 16, which is a 10.9X increase with SKY. Rounding to 56% and 5% results in an 11X increase. The increase has thus been represented as approximately 11% (~11%) on the page. Please be aware and adjust as appropriate per local requirements. |
| * | P<0.001. |
| Period A co-primary endpoints: PASI 90 and sPGA 0/1 at Week 16 (NRI-MI). | |
| sPGA 0/1 at Week 16: SKYRIZI 75%; apremilast 18%; P<0.001. | |
| Dosing: SKYRIZI was dosed 150 mg (one subcutaneous injection) at Week 0, Week 4, and every 12 weeks thereafter. Apremilast was dosed 30 mg (taken orally) twice daily, approximately 12 hours apart. |
| * | One non–treatment-emergent death of unknown cause on study Day 189 that occurred 161 days after the last dose of study drug. |
| † | One patient with sudden cardiac death on study Day 385 (101 days after last dose of study drug; event was not considered to be related to study drug by investigator). |
| ‡ | One patient with type 1 myocardial infarction on study Day 168 (event was not considered to be related to study drug by investigator). |
| * | The most frequently reported infectious adverse events were viral upper respiratory tract infection and upper respiratory tract infection. |
| † | One patient with acute myocardial infarction on study Day 73 (event was not considered to be related to study drug by investigator). |
| ‡ | One patient with stage IV gall bladder cancer. One patient with cholelithiasis underwent gall bladder surgery, had cardiopulmonary arrest, and died due to abdominal abscess, sepsis, and gastric perforation (events were not considered to be study drug related by investigator). |
UltIMMa-1 and UltIMMa-2: Study design
UltIMMa-1 AND UltIMMa-2 STUDY DESIGN vs USTEKINUMAB2
UltIMMa-1 (N=506) and UltIMMa-2 (N=491) were replicate Phase 3 multi-national, 52-week, randomized, double-blind, placebo-controlled, active comparator, controlled trials. Patients 18 years or older with moderate to severe plaque psoriasis were stratified by weight and previous exposure to TNF inhibitor and randomly assigned (3:1:1) to receive subcutaneous risankizumab 150 mg, ustekinumab 45 mg/90 mg (based on weight per label), or placebo.
Dosing occurred at Weeks 0 and 4 (during Part A) and Weeks 16, 28, and 40 (during Part B). Following the 16-week placebo-controlled treatment period (Part A), patients initially assigned to placebo switched to 150 mg of risankizumab at Week 16. Other patients continued double blind with their originally randomized treatment (Part B) for Weeks 16–52.
All efficacy analyses were done in the ITT population.
Co-primary endpoints: Proportion of patients achieving PASI 90 and an sPGA 0/1 at Week 16 (NRI).
IMMerge STUDY DESIGN vs SECUKINUMAB5
Phase 3b, multicenter, randomized, open-label, efficacy assessor-blinded, active-comparator study designed to evaluate the safety and efficacy of SKYRIZI compared to secukinumab in adult patients with moderate to severe plaque psoriasis.
A total of 327 subjects were randomized 1:1 to SKYRIZI (n=164) (150 mg), given as two 75-mg subcutaneous injections at baseline, 4 weeks later, and every 12 weeks thereafter, or secukinumab (n=163) (300 mg) given as two 150-mg subcutaneous injections, at baseline, Weeks 1, 2, 3, and 4, and then every 4 weeks thereafter.
Safety was assessed in all patients.
Baseline characteristics:
Key demographics and baseline characteristics were generally balanced between treatment groups and consistent with the pivotal UltIMMa-1 and UltIMMa-2 trials.
Primary endpoints
• PASI 90 at Week 16 (noninferiority)
• PASI 90 at Week 52 (superiority)
IMMvent PHASE 3 STUDY vs ADALIMUMAB6
A 44-week, randomized comparative study vs adalimumab in adult patients with moderate to severe chronic plaque psoriasis (N=605).
Co-primary endpoints:
• PASI 90 at Week 16
• sPGA 0/1 at Week 16
Primary endpoint after rerandomization: PASI 90 at Week 44 (rerandomized patients)
Secondary endpoints:
• PASI 75 at Week 16
• PASI 100 at Weeks 16 and 44 (rerandomized patients only at Week 44)
Part A (Baseline to Week 16): Patients received either SKYRIZI 150 mg or adalimumab (80 mg at baseline, 40 mg at Week 1, and then once every 2 weeks).
Part B (Weeks 16 to 44): The SKYRIZI group continued on treatment. For the adalimumab group, treatment regimen was dependent on the level of PASI response:
• PASI <50 switched to SKYRIZI
• PASI 50 to <PASI 90 (rerandomized to either SKYRIZI or adalimumab)
• ≥PASI 90 continued with adalimumab
Adalimumab patients who switched to risankizumab in Part B were dosed at Weeks 16, 20, and 32.
IMMpulse STUDY DESIGN vs APREMILAST7
A Phase 4, multicenter, randomized, open-label, efficacy-assessor blinded, active-comparator study to evaluate the efficacy and safety of SKYRIZI compared to apremilast in adult patients with moderate PsO who were candidates for systemic therapy.
Study population: 352 patients with moderate PsO defined as PASI ≥12, BSA 10%-15%, and sPGA=3.
PERIOD A (WEEK 16 DATA) – ENDPOINTS
Co-primary endpoints
• PASI 90
• sPGA 0/1
Ranked secondary endpoint
• PASI 75
Prespecified, nonranked endpoints
• PASI 100
• sPGA 0
PERIOD B (WEEK 52 DATA) – ENDPOINTS
Primary endpoint*
• PASI 90
Ranked secondary endpoints*
• PASI 75
• sPGA 0/1
Prespecified, nonranked endpoints
• PASI 100
• sPGA 0
Period A (baseline to Week 16): Patients received either SKYRIZI 150 mg (1 subcutaneous injection) or apremilast 30 mg orally twice daily (BID).
Period B (Weeks 16-52): The SKYRIZI group continued on treatment. All patients initially randomized to apremilast were rerandomized at Week 16 in a 1:1 ratio to receive either SKYRIZI 150 mg at Weeks 16, 20, 32, and 44 without washout or apremilast 30 mg orally BID up to Week 52. Rerandomization was stratified by PASI 75 response to apremilast (PASI 75 responder, nonresponder) at Week 16.
Rescue with SKYRIZI was offered to patients who were rerandomized to apremilast and were PASI 50 nonresponders at Week 28 or Week 40.
| * | Primary and ranked secondary endpoints in Period B are in patients not achieving PASI 75 response with apremilast at Week 16 in rerandomized patients.7rimary and ranked secondary endpoints in Period B are in patients not achieving PASI 75 response with apremilast at Week 16.7 |
EU INDICATIONS AND IMPORTANT SAFETY INFORMATION ABOUT SKYRIZI (risankizumab)
Indications1
Skyrizi (risankizumab) is indicated for the treatment of moderate to severe plaque psoriasis in adults who are candidates for systemic therapy.
Skyrizi, alone or in combination with methotrexate (MTX), is indicated for the treatment of active psoriatic arthritis in adults who have had an inadequate response or who have been intolerant to one or more disease-modifying antirheumatic drugs (DMARDs).
Skyrizi is indicated for the treatment of adult patients with moderately to severely active Crohn's disease who have had an inadequate response to, lost response to, or were intolerant to conventional therapy or a biologic therapy.
Important Safety Information1
Risankizumab is contraindicated in patients hypersensitive to the active substance or to any of the excipients, and in patients with clinically important active infections (e.g. active tuberculosis). Risankizumab may increase the risk of infection. In patients with a chronic infection, a history of recurrent infection, or known risk factors for infection, risankizumab should be used with caution. Treatment with risankizumab should not be initiated in patients with any clinically important active infection until the infection resolves or is adequately treated.
Patients treated with risankizumab should be instructed to seek medical advice if signs or symptoms of clinically important chronic or acute infection occur. If a patient develops such an infection or is not responding to standard therapy for the infection, the patient should be closely monitored and risankizumab should not be administered until the infection resolves.
Prior to initiating treatment with risankizumab, patients should be evaluated for tuberculosis (TB) infection. Patients receiving risankizumab should be monitored for signs and symptoms of active TB. Anti-TB therapy should be considered prior to initiating risankizumab in patients with a past history of latent or active TB in whom an adequate course of treatment cannot be confirmed.
Prior to initiating therapy with risankizumab, completion of all appropriate immunisations should be considered according to current immunisation guidelines. If a patient has received live vaccination (viral or bacterial), it is recommended to wait at least 4 weeks prior to starting treatment with risankizumab. Patients treated with risankizumab should not receive live vaccines during treatment and for at least 21 weeks after treatment.
If a serious hypersensitivity reaction occurs, administration of risankizumab should be discontinued immediately and appropriate therapy initiated.
The most frequently reported adverse reactions were upper respiratory infections (from 13% in psoriasis to 15.6% in Crohn’s disease). Commonly (≥ 1/100 to < 1/10) reported adverse reactions included tinea infections, headache, pruritus, rash, fatigue, and injection site reactions.
This is not a complete summary of all safety information.
Please see the SmPC for complete prescribing information.
EU INDICATIONS AND IMPORTANT SAFETY INFORMATION ABOUT HUMIRA (adalimumab)
Indications8
Adalimumab is indicated for the treatment of moderate to severe chronic plaque psoriasis in adult patients who are candidates for systemic therapy.
Safety considerations8
Contraindications
Hypersensitivity to adalimumab or any of the excipients, active tuberculosis, or other severe infections, such as sepsis and opportunistic infections, and moderate to severe heart failure (NYHA class Ill/IV) are contraindications to the use of adalimumab.
Serious infections and malignancy
Fatal and life-threatening infections (including sepsis, opportunistic infections, and TB), HBV reactivation, and various malignancies (including leukemia, lymphoma, and HSTCL) have also been reported with use of adalimumab.
Other serious adverse events
Serious adverse reactions have been reported for adalimumab.
TNF-antagonists, such as adalimumab, affect the immune system and their use may affect the body's defense against infection and cancer. Serious hematological, neurological, and autoimmune reactions have been reported in patients treated with adalimumab. These include rare reports of pancytopenia, aplastic anemia, central and peripheral demyelinating events, and reports of lupus, lupus-related conditions, and Stevens-Johnson syndrome.
Most frequent adverse events
The most frequently reported adverse events across all indications include respiratory infections, injection site reactions, headache, and musculoskeletal pain.
Pediatric population
In general, the adverse events in pediatric patients treated with adalimumab were similar in frequency and type to those seen in adult patients.
Vaccinations
It is recommended that pediatric patients, if possible, be brought up to date with all immunizations in agreement with current immunization guidelines prior to initiating adalimumab therapy. Patients on adalimumab may receive concurrent vaccinations, except for live vaccines. The risks and benefits of adalimumab should be carefully considered prior to initiating therapy.
This is not a complete summary of all safety information.
| References: 1. SKYRIZI [Summary of Product Characteristics]. AbbVie Ltd; September 2023. 2. Gordon KB, Strober B, Lebwohl M, et al. Efficacy and safety of risankizumab in moderate-to-severe plaque psoriasis (UltlMMa-1 and UltlMMa-2): results from two double-blind, randomised, placebo-controlled and ustekinumab-controlled phase 3 trials. Lancet. 2018;392(10148):650-661. doi:10.1016/S0140-6736(18)31713-6 3. Blome C, Gosau R, Radtke MA, et al. Patient-relevant treatment goals in psoriasis. 0. 2016;308(2):69-78. doi:10.1007/s00403-015-1613-8 4. Ryan C, Puig L, Zema C, et al. Incremental benefits on patient-reported outcomes for achieving PASI 90 or PASI 100 over PASI75 in patients with moderate to severe psoriasis. Poster presented at: 2018 European Academy of Dermatology and Venereology (EADV) Congress; September 12–16, 2018; Paris, France. Poster 2002. 5. Warren RB, Blauvelt A, Poulin Y, et al. Efficacy and safety of risankizumab vs. secukinumab in patients with moderate-to-severe plaque psoriasis (IMMerge): results from a phase III, randomized, open-label, efficacy assessor-blinded clinical trial. Br J Dermatol. 2021;184(1):50-59. doi:10.1111/bjd.19341 6. Reich K, Gooderham M, Thaçi D, et al. Risankizumab compared with adalimumab in patients with moderate-to-severe plaque psoriasis (IMMvent): a randomised, double-blind, active-comparator-controlled phase 3 trial. Lancet. 2019;394(10198):576-586. doi:10.1016/S0140-6736(19)30952-3 7. Stein Gold LF, Bagel J, Tyring SK, et al. Comparison of risankizumab and apremilast for the treatment of adult patients with moderate plaque psoriasis eligible for systemic therapy: results from a randomised, open-label, assessor-blinded phase IV (IMMpulse) study. Br J Dermatol. 2023;189(5):540-552. doi:10.1093/bjd/ljad252 8. HUMIRA [Summary of Product Characteristics]. AbbVie Deutschland GmbH & Co. KG; October 2022. |
| ADA: adalimumab; APR: apremilast; BID: twice a day; BSA: body surface area; EOW: every other week; IL-12/23i: interleukin-12/23 inhibitor; IL-17i: interleukin-17 inhibitor; ITT: intent-to-treat; MACE: major adverse cardiovascular event; MOA: mechanism of action; NRI: nonresponder imputation; NRI-MI: nonresponder imputation multiple-imputation; PASI: Psoriasis Area and Severity Index; PBO: placebo; PDE4i: Phosphodiesterase-4 (PDE-4) inhibitor; PsO: psoriasis; SAE: serious adverse event; sPGA: static Physician’s Global Assessment; TEAE: treatment-emergent adverse event; TNFi: tumor necrosis factor inhibitor; UST: ustekinumab. |
| [Insert local AbbVie affiliate address] |
| This website is intended for [CountryName] Healthcare Professionals |
| © 2023 AbbVie. All rights reserved. |
| All trademarks are the property of their respective owners. No use of any AbbVie trademark, trade name, or trade dress in this site may be made without the prior written authorization of AbbVie Inc., except to identify the product or services of the company. |
| ALL-SKZD-230116 December 2023 |